Resource Topics: mental health problems


Resources
MythBuster – Trauma and mental health in young people: Let’s get the facts straight
Introduction
Most young people will have been exposed to at least one traumatic event in their lifetime. Multiple and prolonged exposure to trauma is also common. When a young person reaches out to open up about trauma, the way that others around them respond can have a massive impact on the young person’s ability to understand and cope with their experiences. Yet some aspects of trauma remain largely misunderstood, particularly its relationship with mental health.
This mythbuster has been created for young people, their families, and carers to replace some of the most common and harmful myths about trauma in the mental health space with a better understanding of what trauma is and how it can affect young people.
Trauma can come from many different life experiences
What is trauma?
Trauma is broadly described as a deeply distressing experience that can be emotionally, mentally, or physically overwhelming for a person. It takes on many different forms and effects vary from one person to another (van der Kolk et al., 2005; Bryson et al., 2017). It is important to know that an experience does not have to be life threatening to be traumatic. Approximately two thirds of young people will have been exposed to a traumatic event by the time they turn 16 (Copeland et al., 2007). Experiencing a traumatic event can potentially affect both their current and future mental health.
What types of events cause trauma?
Trauma can arise from many different life experiences. Some examples of different types of trauma are listed below:
Direct and indirect trauma
Some types of trauma are called ‘direct trauma’, and others are called ‘indirect trauma’ (May & Wisco, 2016). A ‘direct trauma’ is experienced first-hand or by witnessing a trauma occurring to another person. An ‘indirect trauma’ comes from hearing or learning about another person’s trauma second-hand.
Single event trauma
Single event trauma is related to a single, unexpected event, such as a physical or sexual assault, a fire, an accident, or a serious illness or injury. Experiences of loss can also be traumatic, for example, the death of a loved one, a miscarriage, or a suicide.
Complex trauma
Complex trauma is related to prolonged or ongoing traumatic events, usually connected to personal relationships, such as domestic violence, bullying, childhood neglect, witnessing trauma, emotional abuse, sexual abuse, or torture.
Vicarious trauma
Vicarious trauma can arise after hearing first-hand about another person’s traumatic experiences. It is most common in people working with traumatised people, such as nurses or counsellors. Young people may also experience vicarious trauma through supporting a loved one who is traumatised (e.g. a parent or a friend).
Trans- or intergenerational trauma
Trans- or intergenerational trauma comes from cumulative traumatic experiences inflicted on a group of people, which remain unhealed, and affect the following generations (Hudson, Adams & Lauderdale, 2016). It is most common in young people from refugee or migrant families.
Anyone can experience trauma, regardless of their age or social/cultural background
Who experiences trauma?
Some young people are at higher risk of being victimised, abused, marginalised, excluded, and/or experiencing unsafe situations that leave them vulnerable to potentially traumatic experiences. Young people who are more likely to have experienced trauma include those in out-of-home care, in the juvenile justice system, those experiencing homelessness, young refugees or asylum seekers, and young people working in emergency services (Orygen, 2017). However, it is very important to understand that anyone can experience trauma, regardless of their age or social/cultural background.
How do our perceptions of traumatic events change as we age?
When trying to understand the impact trauma has on the lives of young people, it is important to understand the way we make sense of and respond to trauma as we age. During childhood we are more sensitive to our environment, so how we view threats can be quite different to the way adults view threats (Odgers & Jaffee, 2013). For example, during COVID, parents may be distressed about the safety of their children, the loss of their livelihood, and the impact on their community. On the other hand, children may be most distressed about separation from their extended family and school friends, and the disruption of their daily routines (The Australian Child and Adolescent Trauma Loss and Grief Network, 2010). This can mean that adults might be confused or unable to relate to their child’s response to a traumatic event. Likewise, a child may also be confused by their parents’ reactions and/ or why they might not be feeling or responding to an event in the same way.
Young people and children process trauma differently
As their brains are still developing, children process trauma differently compared to adults. This means that the types of things that children interpret as traumatic, and how they understand them, can be very different to adults.
When looking back at traumatic experiences in childhood, it can be hard to understand the confusing emotions and reactions experienced at the time. A young person might look back and think that they should have been able to understand things ‘better’ or cope ‘better’. This can lead to strong and difficult feelings like anger, guilt, and shame.
When a young person is caught up in this way of thinking, they may cope with an ‘adult’ response. In other words, they attempt to look back on their experiences in childhood through the lens of an adult. By doing this, it is easy to forget that the trauma happened to a child, who has much less ability and life experience, to help them process their trauma and seek support.
The way we make sense of and respond to trauma changes as we age
How does trauma affect young people?
Short-term effects
The short-term effects of trauma are often described as normal reactions to abnormal events (Jones & Wessely, 2007), and can include:
- fear
- guilt
- anger
- isolation
- helplessness
- disbelief
- emotional numbness
- sadness, confusion
- flashbacks or persistent memories and thoughts about the event (van der Kolk, 2000)
It is really important to know that these are normal and healthy reactions to trauma. These can last for up to a month after the trauma has occurred, and can slowly reduce over time.
Long-term effects
Sometimes these strong emotions, thoughts, and memories can continue and even worsen over time. This can overwhelm a young person and have damaging effects on their life and course (e.g. their wellbeing, relationships, and their ability to work and/or study) (Orygen, 2017). Some traumas, such as those occurring in childhood, may have effects that only become clear later in life (Felitti, 2002). In the long-term, there is a strong relationship between trauma and poor mental and/or physical health outcomes; however, in many cases young people can bounce back with the right support (Iacoviello & Charney, 2014; Felitti et al., 1998). Additionally, in some situations, young people can draw personal strength from their struggle with trauma and experience a feeling of positive growth (Meyerson et al., 2011).
Developmental effects
Being exposed to trauma when individuals are very young can change how their brain grows and negatively affect their ability to learn (Whittle et al., 2013; Malarbi er al., 2017). Experiencing high levels of stress at a young age can also increase risk-taking behaviours in adolescence and early adulthood, which can lead to poor physical health later in life (Felitti, 2002).
What is post-traumatic stress disorder or PTSD?
Post-traumatic stress disorder (PTSD) is the most commonly talked about trauma-related diagnosis. Symptoms include having intrusive memories of the traumatic event, increased stress, avoidance of situations and/or people associated with the trauma, and increased negative thoughts (American Psychiatric Society, 2013). These symptoms impact a person’s ability to keep up with their day-to-day life and make it hard for them to focus on work and/or study and other tasks.
In Hong Kong, an increase of people experiencing PTSD symptoms has risen to approximately more than 30% in 2019. PTSD can also cause problems with a person’s relationships with others (Koenen et al., 2017), and symptoms may differ between children, adolescents, and adults (Mikolajewski, Scheeringa & Weems, 2017). Thus, it is really important to get help early if you are struggling to cope after experiencing trauma because evidence shows that the sooner help is sought, the lower the risk of developing PTSD (Gillies et al., 2016).
Evidence shows that the sooner help is sought, the lower the risk of developing PTSD
What are the most common myths about trauma?
Traumatic events and a young person’s reaction to them vary a lot. They can vary between people (e.g. some people may be more sensitive to traumatic experiences than others), within the same person over time, or differ depending on the type of traumatic event the person has experienced.
This can make it difficult for us to have a shared understanding of what trauma is and how it can affect people. If we feel confused or uncertain about what trauma is and how it can affect someone, it would be very easy to end up believing in common and unhelpful myths instead.
Below are some of the common myths surrounding trauma and the reasons why these myths are harmful and untrue.
MYTH: “Everyone who has mental ill-health has experienced trauma”
This myth is particularly harmful because young people who have not experienced trauma, but who are struggling with their mental health may feel that they have no right to feel how they do, or become very confused about how they are interpreting their experiences. They may also worry that if they seek support, everyone would automatically assume they have experienced a type of trauma.
Just because a young person is experiencing mental ill-health, this does not necessarily mean that they have gone through trauma. There are many risk factors that contribute to the beginning of mental ill-health. These can be environmental, genetic, social, and cultural in nature (Kieling et al., 2011).
Mental ill-health can start without a specific event ‘tipping a person over the edge’. In fact, mental ill-health is often triggered by a build-up of a number of smaller stressful events rather than one big traumatic event (Fox & Hawton, 2004). Even though trauma is linked to a higher chance of poor mental health, it is important to remember that the causes of mental ill-health in young people are very complex and differ from person to person (Guina et al., 2017; Paus, Keshavan & Giedd, 2008).
It is really important to know that developing mental health problems after trauma is not a sign of weakness
MYTH: “Everyone who has experienced trauma will develop mental ill-health”
Most people who experience trauma do not develop mental ill-health as a consequence (Sayed, Iacoviello & Charney, 2015). Many factors influence whether or not a young person develops mental ill-health after experiencing trauma. These include the severity and type of trauma, the support available, how easily they can access this support, past traumatic experiences, family history, and physical health (Iacoviello & Charney, 2014; Sayed, Iacoviello & Charney, 2015; Brewin, Andrews & Valentine, 2000).
It is completely normal to experience strong or overwhelming emotions after a traumatic experience, but it is when these symptoms last a long time, worsen overtime, or cause other problems (e.g. using substances to cope) that mental health difficulties are likely to arise. It is really important to know that developing mental health problems after trauma is not a sign of weakness, nor does it reflect anything about you personally. It is simply a sign that you may need some extra support to recover from the effects of your experiences.
MYTH: “It’s my fault”
Trauma can happen to anyone, and if you are a victim of trauma, this does not mean that you are to blame for what happened to you. ‘It’s my fault’ is a common thought after experiencing trauma, and it is completely normal to feel shame, guilt, and/or self-blame after these experiences. Even though you may feel this way, it does not mean you deserve these feelings, and a huge part of recovery is working to overcome them.
These types of emotions are particularly common in young people who have been traumatised by another person (e.g. through sexual abuse, physical abuse, bullying, or violent crime). In cases of trauma resulting from abuse, it is important to understand that abuse comes from the needs and motivations of the perpetrator, not the individual. Being able to work through these strong emotions of self-blame, guilt, and/or shame is essential to recovery. This means it is very important to find the right help to support you through this process.
Traumatic events are sometimes singular and life threatening, but many are more complex.
MYTH: “Only bad things come out of traumatic experiences”
Struggling through traumatic experiences often changes the way a person views the world and people around them. A lot of the time, the changes in thoughts are negative (e.g. the world seems scarier, or people seem less trustworthy). However, in some situations, with the right support, and time to heal, a person may also draw strength and positive change from surviving a traumatic event.
When this happens, it is described as ‘post-traumatic growth’ (Linley & Joseph, 2004; Clay, Knibbs & Joseph, 2009; Tedeschi & Calhoun, 2004). When someone experiences post-traumatic growth, they may gain a greater appreciation for life, a feeling of greater personal strength, a deeper connection to others, and even gain new ideas about the path they see their life taking in the future (Tedeschi & Calhoun, 2004). Research shows that post-traumatic growth is hugely influenced by many psychological, social, and environmental factors in a young person’s life (Meyerson et al., 2011). How each of us reacts to traumatic experiences is deeply linked to these factors, and our different reactions do not make us ‘weaker’ or ‘stronger’ compared to others.
MYTH: “Your life must be threatened for an event to be traumatic”
Traumatic experiences take many different forms (Weiss & Gutman, 2017). There does not have to be one defining event that makes something traumatic. It is true that traumatic events are sometimes singular and life threatening, but others are more complex. Many people experience trauma through ongoing or prolonged exposure to events such as abuse, neglect, and bullying. Others may experience trauma vicariously through encountering another person’s traumatic experiences first-hand.
MYTH: “PTSD is the most common response to trauma”
Although post-traumatic stress disorder (PTSD) is the most commonly talked about trauma-related mental illness, it is not the most common mental health diagnosis among people who have experienced trauma. There are many ways that trauma can affect mental health in young people (Sayed, Iacoviello & Charney, 2015). In fact, for most young people, PTSD only captures a small aspect of their mental health state after trauma (van der Kolk & Courtois, 2005). Young people who have experienced trauma can develop a wide range of mental health problems, without developing PTSD (Odgers & Jaffee, 2013). These can include depression (Widon, Du Mont & Czaja, 2007), anxiety (Fernandes & Osorio, 2015), complex PTSD (Resick et al., 2012), borderline personality disorder (Ball & Links, 2009), substance abuse disorders (Stevens, Murphy & McKnight, 2003), eating disorders (Pignatelli et al., 2017), psychosis (Bendall et al., 2008), and suicide-related behaviours (Miller et al., 2013).
Take home messages
- If you have experienced trauma, you are not alone. Trauma in young people is very common and it is important for family, friends, and mental health professionals to be aware of this.
- Traumatic events can be one off (e.g. car accident, sexual assault), ongoing/prolonged (e.g. childhood sexual abuse, bullying, emotional or physical abuse), or experienced second-hand (e.g. witnessing family violence). Any type of trauma has the potential to be very damaging to a young person’s mental health.
- Often young people who have been abused or neglected feel at blame for what has happened to them – they may feel it was their fault, or that they ‘brought it on’ or ‘asked for it’. If you are in this situation, it is very important to know that you are not to blame, no matter how strong the feelings of guilt or shame may be.
- There is no one uniform or ‘right’ way to respond to a traumatic event. Responses to trauma are highly variable. Different people may react very differently, even to the same situation.
- Young people experiencing mental ill-health have not necessarily experienced trauma, and this does not make their mental health difficulties any less ‘real’ or ‘legitimate’.
- Trauma does not always lead to mental ill-health in young people. Many young people exposed to trauma will make a full recovery without needing mental health intervention.
- Experiencing mental health difficulties related to trauma is not a sign of weakness or failure.
- Trauma can lead to a wide range of mental health difficulties, not just PTSD. These can include anxiety, depression, substance abuse, borderline personality disorder, and eating disorders. It is important to get support from a health professional for any of these difficulties.
- It is possible to recover from mental health difficulties related to trauma.
Help is at hand
Support is a huge protective factor against ongoing mental health difficulties related to trauma. Sometimes people can try to cope with the effects of trauma alone, even though reaching out for support can be hugely beneficial. Some young people might feel an overwhelming sense of self-blame or shame and might not be aware of or understand the effects of trauma, making it even harder to seek support.
Seeking help from someone you know
It is really important to try to find someone you can talk to about what’s going on for you. Seeking support for trauma recovery does not make a person ‘weak’, in fact it is a brave step to take on the road to recovery. Opening up about traumatic events can be daunting, making it very important to find someone you feel comfortable with and can trust to talk to. This person could be a family member, friend, or school counsellor.
Seeking professional help
Some young people may not feel comfortable opening up to people in their personal lives and may prefer to seek help through a mental healthcare professional. In terms of seeking professional help, a good place to start is with your doctor, a counsellor, or through a visit to your closest local support group.
A number of helplines in Hong Kong can be found here:
- Emergency hotline: 999
- The Samaritans 24-hour hotline (Multilingual): (852) 2896 0000
- Samaritan Befrienders Hong Kong 24-hour hotline (Cantonese only): (852) 2389 2222
- Suicide Prevention Services 24-hour hotline (Cantonese only): (852) 2382 0000
- OpenUp 24/7 online emotional support service (English/Chinese): www.openup.hk
More hotlines and resources can also be found here:
Want to know more?
Some helpful resources about trauma and its effects include:
- Asking for Help: When it’s time to talk about your mental health- Coolminds and Charlie Waller Memorial Trust (CWMT) UK factsheet
- Seeking help and what to expect- Coolminds factsheet
- Discrimination and Mental Health: A Guide for Young People- Coolminds factsheet
- Voices of Youth: Stigma, Discrimination and Mental Health- Coolminds factsheet
Supporting someone who has experienced trauma can be emotionally overwhelming, making it equally important to look after yourself. If you are concerned about the wellbeing of someone close to you, it is important to reach out for additional help.
Some highly recommended websites that offer more information on how to support to someone affected by trauma include:
- Samaritans Hong Kong
- Samaritans Befrienders Hong Kong
- The Zubin Foundation- Ethnic Minority Well-being Centre (EMWC)
- Christian Action (Woo Sung Centre)
- Yang Memorial Methodist Social Service- Yau Tsim Mong Family Education and Support Centre
- The Salvation Army Youth, Family and Community Services
- Post Traumatic Stress Disorder – Institute of Mental Health Castle Peak Hospital
- BGCA – What is Trauma?
References
1. van der Kolk, BA, et al. 2005, ‘Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma’, Journal of Traumatic Stress, vol. 18, no. 5. pp. 389–399.
2. Bryson, SA, et al. 2017, ‘What are effective strategies for implementing trauma-informed care in youth inpatient psychiatric and residential treatment settings? A realist systematic review’, International Journal of Mental Health Systems, vol. 11, pp. 36.
3. Copeland, WE, et al. 2007, ‘Traumatic events and posttraumatic stress in childhood’, Archives of General Psychiatry, vol. 64, no. 5, pp. 577–584.
4. Hudson, CC, Adams, S & Lauderdale, J 2016, ‘Cultural expressions of intergenerational trauma and mental health nursing implications for US healthcare delivery following refugee resettlement: an integrative review of the literature’, Journal of Transcultural Nursing, vol. 27, no. 3, pp. 286–301.
5. May, CL & Wisco BE 2016, ‘Defining trauma: how level of exposure and proximity affect risk for posttraumatic stress disorder’, Psychological Trauma, vol. 8, no. 2, pp. 233–40.
6. Orygen The National Centre of Excellence for Youth Mental Health, Youth Mental Health Policy Briefing: Trauma and Youth Mental Health. 2017, Orygen: Melbourne.
7. Odgers, CL & Jaffee SR 2013, ‘Routine versus catastrophic influences on the developing child’, Annual Review of Public Health, vol. 34, no. 1. pp. 29–48.
8. The Australian Child and Adolescent Trauma Loss and Grief Network 2010, ‘How children and young people experience and react to traumatic events’, Australian National University, Canberra.
9. Jones, E & Wessely S 2007, ‘A paradigm shift in the conceptualization of psychological trauma in the 20th century’, Journal of Anxiety Disorders, vol. 21, no. 2, pp. 164–175.
10. van der Kolk, B 2000, ‘Posttraumatic stress disorder and the nature of trauma’, Dialogues in Clinical Neuroscience, vol. 2, no. 1, pp. 7–22.
11. Felitti, VJ 2002, ‘The relationship of adverse childhood experiences to adult health: Turning gold into lead’, Zeitschrift Fur Psychosomatische Medizin Und Psychotherapie, vol. 48, no. 4, pp. 359–369.
12. Iacoviello, BM & Charney DS 2014, ‘Psychosocial facets of resilience: implications for preventing posttrauma psychopathology, treating trauma survivors, and enhancing community resilience’, European Journal of Psychotraumatology, vol. 5.
13. Felitti, VJ, et al. 1998, ‘Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study’, American Journal of Preventive Medicine, vol. 14, no. 4, pp. 245–258.
14. Meyerson, DA, et al. 2011, ‘Posttraumatic growth among children and adolescents: a systematic review’, Clinical Psychology Review, vol. 31, no. 6, pp. 949–964.
15. Whittle, S, et al. 2013, ‘Childhood maltreatment and psychopathology affect brain development during adolescence’, Journal of the American Academy of Child and Adolescent Psychiatry, vol. 52, no. 9, pp. 940–952.
16. Malarbi, S, et al. 2017, ‘Neuropsychological functioning of childhood trauma and posttraumatic stress disorder: a meta-analysis’, Neuroscience & Biobehavioral Reviews, vol. 72, pp. 68–86.
17. American Psychiatric Society 2013, Diagnostic and Statistical Manual of Mental Disorders, 5th edn, American Psychiatric Publishing, Arlington.
18. Koenen, KC, et al. 2017, ‘Posttraumatic stress disorder in the world mental health Surveys’, Psychological Medicine, vol. 47, no. 13, pp. 2260–2274.
19. Mikolajewski, AJ, Scheeringa, MS & Weems, CF 2017, ‘Evaluating diagnostic and statistical manual of mental disorders, fifth edition, posttraumatic stress disorder diagnostic criteria in older children and adolescents,’ Journal of Child and Adolescent Psychopharmacology, vol. 27, no. 4, pp. 374–382.
20. Gillies, D, et al. 2016, ‘Psychological therapies for children and adolescents exposed to trauma’, Cochrane Database Systematic Reviews, vol. 10, pp. Cd012371.
21. Kieling, C, et al. 2011, ‘Child and adolescent mental health worldwide: evidence for action’, The Lancet, vol. 378, no. 9801, pp. 1515-1525.
22. Fox, C & Hawton K 2004, Deliberate self-harm in adolescence, Jessica Kingsley Publishers, London 23. Guina, J, et al. 2017, ‘Should posttraumatic stress be a disorder or a specifier? Towards improved nosology within the DSM categorical classification system’, Current Psychiatry Reports, vol. 19, no. 10, pp. 66
23. Guina, J, et al. 2017, ‘Should posttraumatic stress be a disorder or a specifier? Towards
improved nosology within the DSM categorical classification system’, Current Psychiatry Reports, vol. 19, no. 10, pp. 66
24. Paus, T, Keshavan, M & Giedd, JN 2008, ‘Why do many psychiatric disorders emerge during adolescence?’, Nature Reviews Neuroscience, vol. 9, no. 12, pp. 947-57
25. Sayed, S, Iacoviello, BM & Charney, DS 2015, ‘Risk factors for the development of psychopathology following trauma’, Current Psychiatry Reports, vol. 17, no. 8, pp. 612
26. Brewin, CR, Andrews, B & Valentine, JD 2000, ‘Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults’, Journal of Consulting and Clinical Psychology, vol. 68, no. 5, pp. 748-66
27. Linley, PA & Joseph S 2004, ‘Positive change following trauma and adversity: a review’, Journal of Traumatic Stress, vol. 17, no. 1, pp. 11-21
28. Clay, R, Knibbs, J & Joseph, S 2009, ‘Measurement of posttraumatic growth in young people: a review’, Clinical Child Psychology and Psychiatry, vol. 14, no. 3, pp. 411-22
29. Tedeschi, RG & Calhoun LG 2004, ‘Posttraumatic Growth: Conceptual Foundations and Empirical Evidence’, Psychological Inquiry, vol. 15, no. 1, pp. 1-18
30. Weiss, KJ & Gutman AR 2017, ‘Testifying About Trauma: A Call for Science and Civility’, Journal of the American Academy of Psychiatry and Law, vol. 45, no. 1, pp. 2-6
31. van der Kolk, BA & Courtois CA 2005, ‘Editorial comments: Complex developmental trauma’, Journal of Traumatic Stress, vol. 18, no. 5, pp. 385-388
32. Widom, CS, Du Mont, K & Czaja, SJ 2007, ‘A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up’, Archives of General Psychiatry, vol. 64, no. 1, pp. 49-56
33. Fernandes, V & Osorio FL 2015, ‘Are there associations between early emotional trauma and anxiety disorders? Evidence from a systematic literature review and meta-analysis’, European Psychiatry, vol. 30, no. 6, pp. 756-764
34. Resick, PA, et al. 2012, ‘A critical evaluation of the complex PTSD literature: implications for DSM-5’, Journal of Traumatic Stress, vol. 25, no. 3, pp. 241-251
35. Ball, JS & Links PS 2009, ‘Borderline personality disorder and childhood trauma: evidence for a causal relationship’, Current Psychiatry Reports, vol. 11, no. 1, pp 63-68
36. Stevens, SJ, Murphy, BS & McKnight, K 2003, ‘Traumatic stress and gender differences in relationship to substance abuse, mental health, physical health, and HIV risk behavior in a sample of adolescents enrolled in drug treatment’, Child Maltreatment, vol. 8, no. 1, pp. 46-57
37. Pignatelli, AM, et al. 2017, ‘Childhood neglect in eating disorders: A systematic review and metaanalysis’, Journal of Trauma and Dissociation, vol. 18, no.1, pp. 100-115
38. Bendall, S et al. 2008, ‘ Childhood trauma and psychotic disorders: a systematic, critical review of the evidence’, Schizophrenia Bulletin, vol. 34, pp. 568-579
39. Miller, AB, et al. 2013, ‘The Relation Between Child Maltreatment and Adolescent Suicidal Behavior: A Systematic Review and Critical Examination of the Literature’, Clinical Child and Family Psychology Review, vol. 16, no. 2, pp. 146-172
Disclaimer
This information is not medical advice. It is generic and does not take into account your personal circumstances, physical wellbeing, mental status or mental requirements. Do not use this information to treat or diagnose your own or another person’s medical condition and never ignore medical advice or delay seeking it because of something in this information. Any medical questions should be referred to a qualified healthcare professional. If in doubt, please always seek medical advice.
Mythbuster writers
Anna Farrelly-Rosch
Dr Faye Scanlan
Youth contributors
Sarah Langley – Youth Research Council
Somayra Mamsa – Youth Research Council
Roxxanne MacDonald – Youth Advisory Council
Clinical consultant
Dr Sarah Bendall
First published as ‘Trauma and mental health in young people: Let’s get the facts straight’ by Orygen, 2018.

Resources
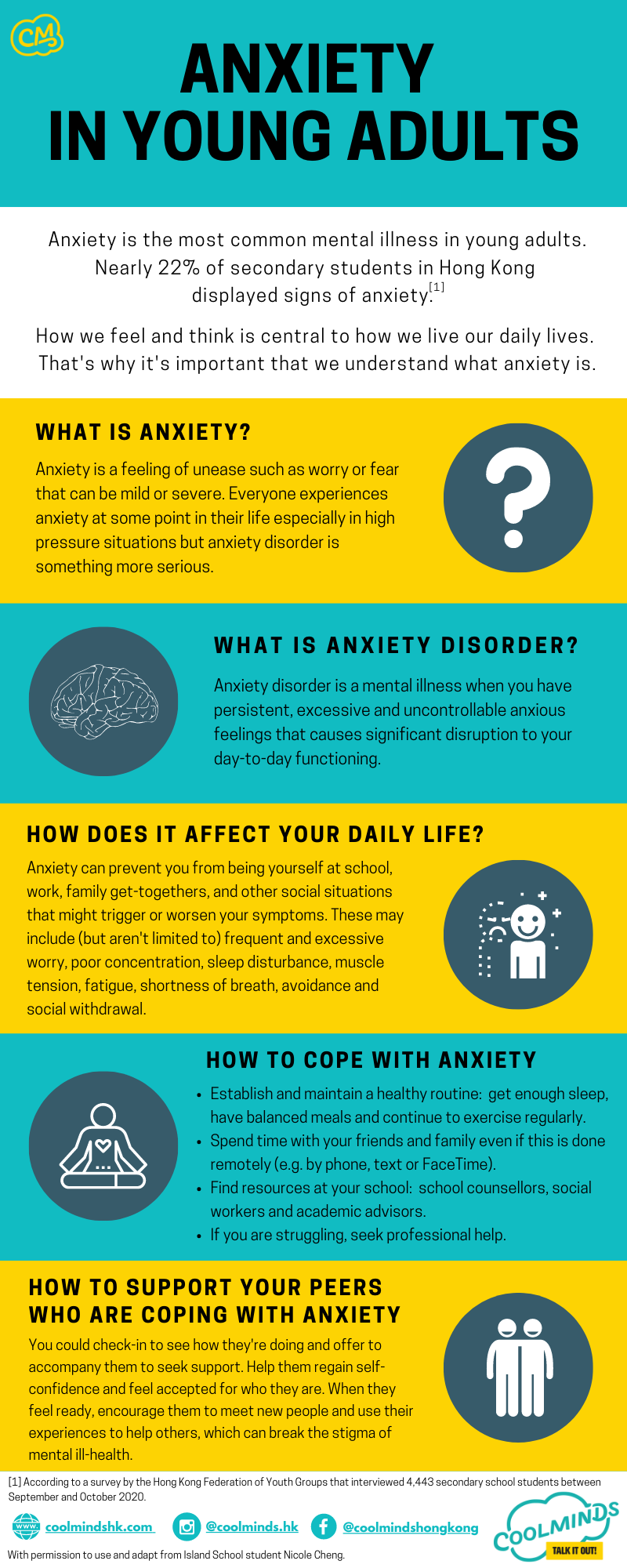
Anxiety in Young Adults
Anxiety is the most common mental illness in young adults.
According to a survey by the Hong Kong Federation of Youth Groups that interviewed 4,443 secondary school students between September and October 2020, nearly 22% of secondary students in Hong Kong displayed signs of anxiety.
How we feel and think is central to how we live our daily lives. That’s why it’s important that we understand what anxiety is.
What is anxiety?
Anxiety is a feeling of unease such as worry or fear that can be mild or severe. Everyone experiences anxiety at some point in their life especially in high pressure situations but anxiety disorder is something more serious.
What is anxiety disorder?
Anxiety disorder is a mental illness when you have persistent, excessive and uncontrollable anxious feelings that causes significant disruption to your day-to-day functioning.
How does it affect your daily life?
Anxiety can prevent you from being yourself at school, work, family get-togethers, and other social situations that might trigger or worsen your symptoms. These may include (but aren’t limited to) frequent and excessive worry, poor concentration, sleep disturbance, muscle tension, fatigue, shortness of breath, avoidance and social withdrawal.
How to cope with anxiety?
- Establish and maintain a healthy routine: get enough sleep, have balanced meals and continue to exercise regularly.
- Spend time with your friends and family even if this is done remotely (e.g. by phone, text or FaceTime).
- Find resources at your school: school counsellors, social workers and academic advisors.
- If you are struggling, seek professional help.
How to support your peers who are coping with anxiety?
You could check-in to see how they’re doing and offer to accompany them to seek support. Help them regain self-confidence and feel accepted for who they are. When they feel ready, encourage them to meet new people and use their experiences to help others, which can break the stigma of mental ill-health.
Special thanks to Island School student Nicole Cheng who granted permission to use and adapt her work.

Resources
Seeking Help and What to Expect
Who to seek help from
Congratulations! If you are reading this section, that means you’re ready for change. But we know that seeking help can be confusing and overwhelming so let’s start by understanding what different mental health professionals do and how they can help. Here’s a guide on the range of mental health professionals that you may find:
General practitioner (GP)
General practitioners, also known as family doctors, are medical doctors specializing in general medicine. They are also the doctors you see when you are feeling physically unwell. Your GP is often the first professional you would see when you are struggling with your mental health. They are trained to assess, diagnose and treat mild to moderate mental health conditions. GP’s can prescribe medications and provide preventative care and health education. They can also refer and direct you to the appropriate specific mental health professionals. Seeing your GP is the best first step to getting help.
Psychiatrists
Psychiatrists are licensed medical doctors who specialize in mental health. They are trained to assess, diagnose and treat mental health disorders, primarily through prescribing and monitoring medication treatment, they often do not provide “talk therapy”. Your visit with a psychiatrist may include a blood test, a physical assessment and a risk assessment. Psychologists can work at hospitals, private offices, or community health centres.
Mental health nurse
A psychiatric nurse is a registered nurse with specialised training in mental health. A psychiatric nurse assesses, supports and advocates for care. They typically assist and work with psychiatrists working in the public health care system. As part of their role they follow up with patients regarding medications, and needed supports.
Social workers
Social workers are dedicated to helping people navigate and solve issues in their lives which may be caused by relationship problems, adjustment issues, traumatic events, or disabilities, etc. Through case management, they redirect clients to resources that best support them. Social workers can be found in a variety of settings, such as schools, private offices, hospitals, community health centres, and non-profit organisations.
Counsellors
Counsellors are masters-level professionals. They aim to help people to understand the complex social welfare system and help to access resources which support a person’s wellbeing. They also receive basic counselling training and may be able to provide counselling to people in distress. Counsellors can be found at schools, hospitals, community health centres, and in private practice.
So what’s the difference between a counsellor and a psychologist?
Psychologists often have more formal education who are trained to diagnose and treat specific mental illnesses, whereas counsellors help people to process and cope with their mental health struggles.
Clinical psychologists
In general, psychologists have doctoral training qualifications; however, they are not medical doctors and do not prescribe medication. Clinical psychologists are specially trained to diagnose and treat mental illnesses through talk therapy, and they are the most common type of psychologist you would see for a mental health issue.
Educational psychologists
Educational psychologists are trained in teaching and education, focusing on learning-related issues. They work with students, parents, teachers, and support professionals to help students in the school setting. Psychologists can be found in places such as private offices, hospitals, and schools.
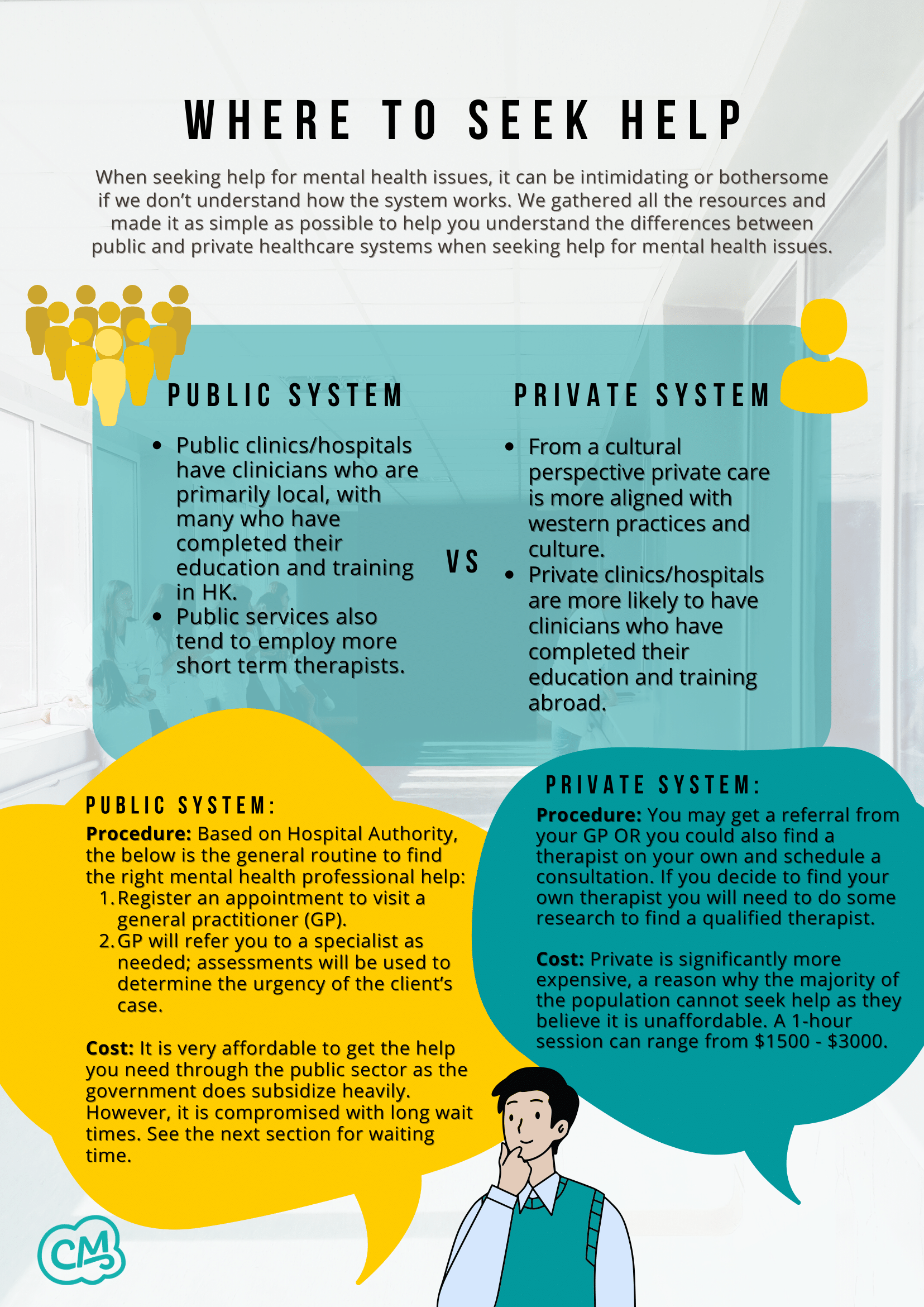
Where to seek help
When seeking help for mental health issues, it can be intimidating or bothersome if we don’t understand how the system works. We gathered all the resources and made it as simple as possible to help you understand the differences between public and private healthcare systems when seeking help for mental health issues.
Public system
- Public clinics/hospitals have clinicians who are primarily local, with many who have completed their education and training in HK.
- Public services also tend to employ more short term therapists.
- Procedure: Based on Hospital Authority, the below is the general routine to find the right mental health professional help:
- Register an appointment to visit a general practitioner (GP).
- GP will refer you to a specialist as needed; assessments will be used to determine the urgency of the client’s case.
- Cost: It is very affordable to get the help you need through the public sector as the government does subsidise heavily. However, it is compromised with long wait times. See the next section for waiting time.
Private system
- From a cultural perspective private care is more aligned with western practices and culture.
- Private clinics/hospitals are more likely to have clinicians who have completed their education and training abroad.
- Procedure: You may get a referral from your GP OR you could also find a therapist on your own and schedule a consultation. If you decide to find your own therapist you will need to do some research to find a qualified therapist.
- Cost: Private is significantly more expensive, a reason why the majority of the population cannot seek help as they believe it is unaffordable. A 1-hour session can range from $1500 – $3000.
What to expect
So what should I expect before I head for my first session?
Before you head to your first session, remember this initial visit to a professional is no different than a first appointment with a new general practitioner (or family doctor). It may be uncomfortable to talk about some of your concerns and experiences but it is an important first step to getting better.
What will we talk about during first session?
However, a small detail that could cause anxious feelings is the fact that your relationship with a therapist is important to help your recovery journey. It could be intimidating to spill all your deepest and “darkest” secrets to a stranger you barely know and the thought of bailing might even cross your mind. Just know that every therapist actually understands the nerves of your feelings and they’ll try their best to soothe you and make you feel comfortable. Regardless, whether you’re full of nerves or can’t wait to start blabbing away on that couch, your new therapist will be ready for you and perfectly able to meet you where you’re at. And if all you want to talk about during that first session is how nervous you are or how much you don’t want to be there, then that’s totally fine.
How does talking with a professional help my condition?
There are many types of “talk therapies” available depending on the mental health issues you are struggling with. One of the most commonly used one is Cognitive Behaviour Therapy (CBT), which focuses on challenging and changing unhelpful thought and behaviour patterns, while improving emotional regulation and developing helpful coping strategies.
So what will happen in the first session?
In your first session, you may be asked about:
- Your mood, thoughts and behaviours
- Your lifestyle (friendships, school, intimate relationships, family relationships)
- Any recent events in your life that might be affecting your wellbeing
- Any changes to your sleep, diet and daily activities
- Your medical history
- If you are seeing a GP or a psychiatrist they may take your blood pressure, listen to your heart, as well as doing blood tests to explore any physical issues that may contribute to your emotions and behaviours
What about with a specific mental health professional? What questions do they ask?
With a specific mental health professional you may be asked:
- How long have you been experiencing these problems or issues?
- What have you tried to do to cope with it?
- What do you think the trigger could be?
- How often are you suffering from it?
- What was your life like before this issue or problem was present?
Are there any other questions they would ask? What should I do if I don’t want to answer certain questions?
There are many other questions that a therapist will ask once you start talking about your presenting problem. They’ll start out pretty general and get more detailed as the sessions move forward.
You’ll be asked to think about what’s going on and how you’re experiencing it. Some of it will feel really personal. A therapist needs to try to understand the triggers and causes of your struggles in order to figure out how they can help. If you ever feel like you don’t want to answer a question quite yet, speak up and say so.
With certain types of therapies or cases it may involve some homework. Just be aware that often therapy is most effective when you also put in the work outside of the office as well.
Often, a therapist will ask you what your goal is for therapy. It’s helpful to figure that out upfront. But it’s also okay if you don’t have a specific goal in mind when you start. There won’t be any pressure to try and define it early on.
- Types of therapy
- Confidentiality
- Your conversations with your therapist are confidential. However, if they are concerned about your safety or the safety of others they will talk to you about disclosing to a trusted supporter (usually your parent/guardian if that is safe).
- Goals of therapy
- Give you the tools and strategies for navigating whatever is going on in your life — from stress or relationship issues to managing a mental health diagnosis
- Process of therapy journey
- Length of treatment
- Touch on it may get worse before it gets better
- Mention every case is different, just because you are diagnosed with a psychological disorder does not indicate you can be generalised and treated like any other client that has the same condition as you.
- Relapse
- We don’t expect recovery to happen overnight, and sometimes it’ll bounce back, making you think you haven’t made any progress. But this is certainly not the case. One thing we want you to take away from reading this booklet is to take the first step of speaking up and seeking help.
Emergency support
If you are experiencing strong levels of distress or trauma which are interfering with your life, remember that you do not have to face it alone, and that help is available.
For emergency support, please contact the hotlines below:
Emergency hotline: 999
The Samaritans 24-hour hotline (Multilingual): (852) 2896 0000
Samaritan Befrienders Hong Kong 24-hour hotline (Cantonese only): (852) 2389 2222
Suicide Prevention Services 24-hour hotline (Cantonese only): (852) 2382 0000
OpenUp 24/7 online emotional support service (English/Chinese): www.openup.hk
More support services can be found here: https://www.coolmindshk.com/en/emergency-hotlines/
More non-urgent support services can be found here: https://www.coolmindshk.com/en/communitydirectory/

Resources
Signs of Depression
We would like to acknowledge the Charlie Waller Memorial Trust (CWMT) UK for these resources and for allowing us to adapt this. For the original version of this resource, please refer to the CWMT website: www.cwmt.org.uk


Resources
Bipolar Disorder Symptoms
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to the Black Dog Institute for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to the Black Dog Institute’s website: www.blackdoginstitute.org.au
What this fact sheet covers:
- What is bipolar disorder
- Sub-types of bipolar disorder
- Symptoms of bipolar disorder
- When to seek help for bipolar disorder
- Key points to remember
- Where to get more information
What is bipolar disorder?
- Bipolar disorder is the name used to describe a set of ‘mood swing’ conditions, the most severe form of which used to be called ‘manic depression’.
- The term describes the exaggerated swings of mood, cognition and energy from one extreme to the other that are characteristic of the illness.
- People with this illness suffer:
- Recurrent episodes of high, or elevated moods (mania or hypomania) and depression.
- Most experience both the highs and the lows.
- Occasionally people can experience a mixture of both highs and lows at the same time, or switch during the day, giving a ‘mixed’ picture of symptoms.
- A very small percentage of sufferers of bipolar disorder only experience the ‘highs’.
People with bipolar disorder experience normal moods in between their mood swings.
- The mood swings pattern for each individual is generally quite unique, with some people only having episodes of mania once a decade, while others may have daily mood swings.
- Bipolar disorder can commence in childhood, but onset is more common in the teens or early 20’s.
- Some people develop ‘late onset’ bipolar disorder, experiencing their first episode in mid-to-late adulthood.
Distinguishing between bipolar I and bipolar II
- Bipolar I disorder is the more severe disorder, in the sense that individuals are more likely to experience ‘mania’, have longer ‘highs’ and to have psychotic episodes and be more likely to be hospitalised.
- Mania refers to a severely high mood where the individual often experiences delusions and/ or hallucinations. The severe highs which are referred to as ‘mania’ tend to last days or weeks.
- Bipolar II disorder is defined as being less severe, in that there are no psychotic features and episodes tend to last only hours to a few days; a person experiences less severe highs which are referred to as ‘hypomania’ and depression but no manic episodes and the severity of the highs does not usually lead to hospitalisation.
- Hypomania literally translates into ‘less than mania’. It describes a high that is less severe than a manic episode and without any delusions and/or hallucinations.
- These highs don’t last as long. While they are officially diagnosed after a four-day duration, research has shown that they may only last a few hours to a few days.
- Both women and men develop bipolar I disorder at equal rates, while the rate of bipolar II disorder is somewhat higher in females.
Symptoms of bipolar disorder
- Diagnosing bipolar disorder is often not a straightforward matter.
- Many people go for 10 years or more before their illness is accurately diagnosed.
- It is important to note that everyone has mood swings from time to time. It is only when these moods become extreme and interfere with a person’s personal and professional life that bipolar disorder may be indicated and medical assessment sought.
- There are two starting points for considering whether you might have bipolar disorder.
- Firstly, you must have had episodes of clinical depression.
- Secondly, you must have had ‘highs’, where your mood was more ‘up’ than usual, or where you felt more ‘wired’ and ‘hyper’.
- If both depression and ‘highs’ have been experienced, then the next thing to consider is whether you also experienced any of the six key features of mania and hypomania outlined below.
Key features of mania & hypomania
While it can be difficult to identify what separates normal ‘happiness’ from the euphoria or elevation that is seen in mania and hypomania, researchers at the Black Dog Institute, have identified the following distinguishing features:
- High energy levels – feeling ‘wired’ and ‘hyper’, extremely energetic, talking more and talking over people, making decisions in a flash, constantly on the go and feeling less need for sleep.
- Positive mood – feeling confident and capable, optimistic that one can succeed in everything, more creative, happier, and feeling ‘high as a kite’.
- Irritability – irritable mood and impatient and angry behaviours.
- Inappropriate behaviour – becoming over involved in other peoples’ activities, engaging in increased risk taking (i.e. by over indulging in alcohol and drugs and gambling excessively) saying and doing outrageous things, spending more money, having increased libido; dressing more colourfully and with disinhibition.
- Heightened creativity – ‘seeing things in a new light’, seeing things vividly and with crystal clarity, senses are heightened and feeling quite capable of writing the ‘next great novel’.
- Mystical experiences – believing that there are special connections between events, that there is a higher rate of coincidence between things happening, feeling at one with nature and appreciating the beauty and the world around, and believing that things have special significance.
- More extreme expressions of mania (but not hypomania) may have the added features of delusions and hallucinations.
- A number of other symptoms can indicate whether there is a likely diagnosis of bipolar disorder, particularly for those under the age of 40. These include:
- Racing thoughts (for example, feeling like you are watching a number of different TV channels at the same time, but not being able to focus on any)
- Sleeping a lot more than usual
- Feeling agitated, restless and/or incredibly frustrated.
When to seek help for bipolar disorder
- If you have experienced an episode of mania or hypomania, or have taken the Black Dog Institute’s Bipolar Disorder Self-Test, linked under the resources at the end of this fact sheet, and are concerned about your results, it is advisable to seek professional assessment by a mental health practitioner.
- The first step is to arrange a consultation with your doctor. They will provide an assessment and, where necessary, refer you to a psychiatrist for further treatment.
- Bipolar disorder is not an illness which goes away of its own accord, but one which often needs long-term treatment. Accurately diagnosing bipolar disorder is a task for the mental health professional.
- Some people with bipolar disorder can become suicidal. It is very important that talk of suicide be taken seriously and for such people to be treated immediately. In an emergency you can go straight to your local hospital’s emergency department for help, or dial 999.
Key points to remember
- Bipolar disorder is an illness involving exaggerated swings of mood and energy from one extreme to the other, usually involving alternating periods of depression and mania or hypomania.
- The pattern of mood swings for each individual is quite unique.
- The six features of mania and hypomania are:
- High energy levels
- Positive mood
- Irritability
- Inappropriate behaviour
- Heightened creativity
- Mystical experiences
- For people under the age of 40, other symptoms of bipolar disorder may include sleeping a lot more than usual, feeling agitated, restless and/or incredibly frustrated.
- Accurately diagnosing bipolar disorder is a task for a skilled mental health practitioner.
- If symptoms of bipolar disorder are suspected it’s best to first see a doctor, who will likely refer you to a psychiatrist.
- People with bipolar disorder can become suicidal. Talk of suicide should be taken seriously and immediate help should be sought from a doctor or other mental health professional.
Contact Us
Coolminds
Email: hello@coolmindshk.com
Black Dog Institute
Email: blackdog@blackdog.org.au
Where to get more information and support
Black Dog Institute – “Bipolar Disorder Self-Test”
Mind Hong Kong – “What Is Bipolar Disorder?”
Bilingual Telephone Hotlines
Hospital Authority Mental Health 24-hour Hotline: 2466 7350
Social Welfare Department Hotline: 2343 2255
Chinese-Only Telephone Hotlines
Youth Outreach 24-hour hotline service: 90881023
The Hong Kong Federation of Youth Groups “Youthline” hotline (available Mon-Sat, 2pm-2am): 27778899

Resources
Signs & Symptoms of Anxiety
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to the Black Dog Institute for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to the Black Dog Institute’s website: www.blackdoginstitute.org.au
What this fact sheet covers:
- When anxiety is a problem
- Types of anxiety disorders
- Signs and symptoms of anxiety
Everyone experiences anxiety
Feeling anxious in certain situations can help us avoid danger, triggering our ‘fight or flight’ response. Sometimes though, we can become overly worried about perceived threats – bad things that may or may not happen. When your worries are persistent or out of proportion to the reality of the threat, and get in the way of you living your life, you may have an anxiety disorder.
In Hong Kong,
- Over half of the university students show symptoms of an anxiety disorder, according to research conducted by the University of Hong Kong in 2016
- According to a 2018 survey by Hong Kong Playground Association, over a third of young people scored moderate to extremely severe on the Anxiety scale (of the DASS21)
When does anxiety become a problem?
It’s normal to feel anxious in high pressure situations such as:
- A job interview
- When you’re speaking in public
- When you’re experiencing change in your life or work environment and you’re uncertain what the future will hold.
To a degree, this anxiety can help us, making us stay focused and alert.
When we’re very anxious, we have intense feelings of worry or distress that are not easy to control. Anxiety can interfere with how we go about our everyday lives making it hard to cope with ‘normal’ challenges.
Anxiety becomes a problem when you start to feel anxious most of the time and about even minor things, to the point where your worry is out of control and interfering with your day to day life.
What are anxiety disorders?
Anxiety disorders are a mix of:
- Psychological symptoms: frequent or excessive worry, poor concentration, specific fears or phobias e.g. fear of dying or fear of losing control
- Physical symptoms: fatigue, irritability, sleeping difficulties, general restlessness, muscle tension, upset stomach, sweating and difficulty breathing
- Behavioural changes: including procrastination, avoidance, difficulty making decisions and social withdrawal
Severe anxiety is a feature of a group of mental health disorders including:
- Generalised anxiety disorder
- Social phobia
- Specific phobia
- Obsessive compulsive disorder (OCD)
- Panic disorder
- Separation anxiety disorder
- Agoraphobia
- Post-traumatic stress disorder (PTSD)
Other types of anxiety disorders include:
- Substance/medication-induced anxiety disorder
- Anxiety disorder due to a medical condition
It’s important to seek help to manage severe anxiety. There are many effective treatments for anxiety, and you can feel better.
Factors for developing anxiety
There is a range of contributing factors for developing anxiety. The factors could be:
- Biological – genes (family history)
- Personality traits
- Brain chemistry
- Life events, such as trauma and long-term stress
- A combination of above factors
Signs and symptoms
While there are many types of anxiety disorder, there are some common signs and symptoms.
You might be feeling:
- Very worried or afraid most of the time
- Tense and on edge
- Nervous or scared
- Panicky
- Irritable, agitated
- Worried you’re going crazy
- Detached from your body
- Feeling like you may vomit
You may be thinking:
- ‘Everything’ is going to go wrong’
- ‘I might die’
- ‘I can’t handle the way I feel’
- ‘I can’t focus on anything but my worries’
- ‘I don’t want to go out today’
- ‘I can’t calm myself down’
You may also be experiencing:
- Sleep problems (can’t get to sleep, wake often)
- Pounding heart
- Sweating
- ‘Pins and needles’
- Tummy aches, churning stomach
- Lightheadedness, dizziness
- Twitches, trembling
- Problems concentrating
- Excessive thirst
When these constant repetitive thoughts and feelings take over, we can:
- Feel overwhelmed
- Lose sleep
- Feel exhausted
- Start to avoid social situations
Some of these symptoms can also be signs and symptoms of other medical conditions, so it’s always best to see a doctor so they can check them properly.
There is an online Anxiety Self-test on the Black Dog Institute website.
Diagnosis
To be diagnosed with an anxiety disorder, a combination of symptoms
- Is present on most days for more than six months
- Interferes with your ability to function at work or at home
It is common to experience a low mood secondary to excessive worry and the two conditions – clinical depression and anxiety disorder – can occur at the same time.
It’s important to get help to treat anxiety disorders. Left untreated, anxiety can last for a long time. It can become exhausting, debilitating and get in the way of us living our everyday lives. There are a range of effective treatments for anxiety, and you can get better. Visiting a doctor or a mental health professional is a good starting point when seeking help for anxiety.
Key points to remember
- Anxiety is normal, everyone experiences anxiety at some time.
- Anxiety becomes a problem when it interferes with your day to day life
- Anxiety disorders are a combination of psychological, physical and behavioural symptoms
- A range of factors can contribute to anxiety disorders
- Signs and symptoms of anxiety vary
Contact Us
Coolminds
Email: hello@coolmindshk.com
Black Dog Institute
Email: blackdog@blackdog.org.au

Resources
Seeking Help for Anxiety
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to the Black Dog Institute for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to the Black Dog Institute’s website: www.blackdoginstitute.org.au
What this fact sheet covers:
- Why seek help for anxiety?
- Who to talk to
- Treatment available
It’s important to get treatment for anxiety
Anxiety is physically and emotionally exhausting. Getting help early means you can start to get relief and recover sooner. There are many professionals who treat all kinds of anxiety.
There is a wide range of effective treatments for anxiety, e.g.
- Cognitive behavioural therapy (CBT)
- E-mental health tools
- Relaxation techniques
- Medications
There are also lots of things you can do to help yourself.
Often, it’s a combination of things that help us get better, such as:
- A well-informed health professional you feel comfortable talking to
- The right psychological and medical therapies
- Support from family and friends
- Exercising and healthy eating
- Learning ways to manage challenges and stress, such as structured problem solving, meditation and yoga
How do I know it’s anxiety?
Severe anxiety can appear in ways that feel like other health issues, e.g.
- Chest pain
- A racing heartbeat
- Dizziness
- Rashes
Sometimes, anxious people think they’re having a heart attack.
When we’re anxious, we can also become hyper-aware of:
- Our body
- Aches and pains
- Perceived threats and danger
Sometimes, once we’re aware of a problem, we can become ‘hyper-vigilant’ in checking on all the discomforts and pains we feel. This can spiral into feeling more concern and worry, making the anxiety more severe.
You should always see a doctor, so they can make a thorough check of your symptoms and rule out any other medical condition.
Who can provide help for anxiety?
As well as your doctor, there are other health professionals who can help with anxiety, including:
- Psychologists
- Psychiatrists
- Counsellors
- School and university counsellors
- Social workers and occupational therapists trained in mental health
- Mental health nurses
What type of treatment is available?
There are three broad categories of treatment for anxiety:
- Psychological treatments (talking therapies)
- Physical treatments (medications)
- Self-help and alternative therapies
Psychological therapies are the most effective way to treat and prevent the recurrence of most types of anxiety. Depending on the type of anxiety, self-help and alternative therapies can also be helpful. They can be used alone or combined with physical and psychological treatments.
A thorough assessment by your doctor is needed to decide on the best combination of treatments for you.
Psychological treatments
Psychological treatments can be one-on-one, group-based or online interactions. Psychological treatments are sometimes called ‘talking therapies’ as opposed to ‘chemical therapies’ (i.e. medications).
Talking therapies can help us change habits in the way we think, and cope better with life’s challenges. They can help us address the reasons behind our anxiety, and also prevent anxiety from returning.
There are a wide range of psychological treatments for anxiety, including:
- Cognitive behaviour therapy (CBT)
- Exposure therapy (behaviour therapy)
- Interpersonal therapy (IPT)
- Mindfulness-based cognitive therapy
- Positive psychology
- Psychotherapies
- Counselling
- Narrative therapy
Some of the above treatments can be accessed online. Evidence-based online treatments can be as effective as face-to-face treatments. These online treatments are often referred to as e-mental health programs.
Physical treatments
Your doctor should undertake a thorough health check before deciding whether medication is a good option for you. Taking medication for anxiety must be supervised by a doctor. If medication is prescribed as part of your treatment, your doctor should explain the reason for choosing the medication they’ve prescribed.
Your doctor will:
- Discuss the risks and benefits, side effects, and how regularly you need check-ups.
- Advise what treatments can work together with the medication, such as psychotherapy, lifestyle changes (e.g. exercise) and other support options.
Anti-anxiety medications are used for very severe anxiety in anxiety types such as:
- Panic disorder
- Generalised anxiety disorder (GAD)
- Social phobia
Anti-anxiety medications, such as benzodiazepines, can:
- Be addictive
- Become ineffective over time
- Have other side effects such as headaches, dizziness and memory loss
Anti-anxiety medications are not recommended for long-term use.
It’s important to know that not all anxiety needs medication. Many people respond well to lifestyle changes and psychological treatments.
Self-help and alternative therapies
There are a wide range of self-help measures and therapies that can be useful for anxiety. It’s good to know that there are things you can do for yourself to feel better.
Self-help and complementary therapies that may be useful for anxiety include:
- Exercise
- Good nutrition
- Omega-3
- Meditation
- De-arousal strategies
- Relaxation and breathing techniques
- Yoga
- Alcohol and drug avoidance
- Acupuncture
Different types of anxiety respond to different kinds of treatments. Severe anxiety may not respond to self-help and alternative therapies alone. These can be valuable adjuncts to psychological and physical treatments.
e-mental health programs
e-mental health programs can be used in conjunction with a mental health professional or as a stand-alone option. e-mental health programs (also called ‘e-therapies’ or ‘online therapies’) are online mental health treatment and support services. You can access them on the internet using your smartphone, tablet or computer. The programs can help people experiencing mild-to- moderate depression or anxiety.
Some e-mental health tools, such as myCompass developed by the Black Dog Institute, have been found to be as effective in treating mild-to- moderate depression as face-to-face therapies.
e-mental health treatments are based on face-to-face therapy, positive psychology and behavioural activation. These therapies mainly focus on reframing thoughts and changing behaviour.
Key points to remember
- Lots of professionals can help you with anxiety
- There are many types of treatments for anxiety, and you can get better
- Many people who have had anxiety have been able to seek help and live active, fulfilling lives
Contact Us
Coolminds
Email: hello@coolmindshk.com
Black Dog Institute
Email: blackdog@blackdog.org.au
Where to get more Information and Support
Black Dog Institute – “myCompass”
Student Health Services – “Understanding Anxiety Disorders”
OCD & Anxiety Support Hong Kong
Mind Hong Kong – “Anxiety and Panic Attacks”
The Mental Health Association of Hong Kong:
Phone: 2528 0196
Website: www.mhahk.org.hk

Resources
Helping Someone Who Has a Mental Illness: For Family and Friends
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to the Black Dog Institute for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to the Black Dog Institute’s website: www.blackdoginstitute.org.au
What this fact sheet covers:
- How to tell if someone has a mental illness
- What to do if you are concerned about a family member or close friend
- How to behave with someone who is depressed
- What to do if someone is suicidal
- Self care for carers
- Key points to remember
- Further information and support
Someone with a mood disorder is like anyone with any other illness – they need care and support.
Family and friends can provide better care if they are informed about the illness, understand the type of treatment and are aware of the expected recovery time.
How to tell if someone has a mental illness
Even if you know someone well, you will not always notice when they have changed. You are more likely to notice big or sudden changes but gradual changes can be easy to miss. It’s also true that people will not always reveal all their thoughts and feelings to their close friends and family.
For these reasons, family and friends cannot expect to always know when someone has a depressive illness and should not feel guilty that they ‘did not know’.
The best approach is to acknowledge that mental illnesses are common and to learn how to recognise the signs and how to offer help.
What to do if you are concerned about a family member or close friend
If you are worried that a family member or close friend has a mood disorder, try talking to them about it in a supportive manner and either suggest that they consult their doctor or another mental health professional.
Sometimes they may be reluctant to seek help. You might need to explain why you’re concerned and provide specific examples of their actions or behaviour that are worrying you. Providing them some information such as a book, fact sheets or helpful pamphlets might also help.
You could offer to assist them in seeking professional help by:
- Finding someone that they feel comfortable talking to.
- Making an appointment for them on their behalf.
- Taking them to the appointment on the day
- Accompanying them during the appointment if appropriate.
This level of help may be particularly appropriate if the person has a severe mood disorder such as psychotic depression or mania.
Young people, adolescents in particular, are vulnerable to mental health problems. If you are concerned about someone, try:
- Gently let them know you have noticed. changes and explain why you are concerned
- Find a good time to talk when there are no pressures or interruptions.
- Listen and take things at their pace
- Respect their point of view.
- Validate what they are experiencing, but don’t offer reassurance or advice too quickly
- Let them know that there is help available that will make them feel better.
- Encourage them to talk to a doctor or other health professional, and to find a trusted friend or family member that they can confide in.
There are also a range of services (e.g. telephone counselling and online resources) that are specifically designed for young people. You can find out more about what is provided in Hong Kong on the Coolminds website.
How to behave with someone who is depressed
Patience, care and encouragement from others are vital to a person who is experiencing depression. Someone experiencing depression is very good at criticising themselves and needs support from others, not criticism.
Clear and effective communication within the household or family is also important. Partners or families might find it helpful to see a psychologist during this time for their own support.
An episode of depression can provide an opportunity for family members to re-evaluate the important things in life and resolve issues such as grief or relationship difficulties.
Some Tips:
- Avoid suggesting to the person that they “cheer up” or “try to get over it”. This is unhelpful as it is likely to reinforce their feelings of failure or guilt.
- Another important part of caring is to help the treatment process – if medication has been prescribed, encourage the person to persist with treatment and to discuss any side effects with their prescribing doctor.
- The person may also need encouragement and help to get to their therapy appointments or complete any online therapy exercises they have been asked to do.
- During a depressive illness, counselling or psychotherapy often results in the person working through their life events and relationships; while this can be difficult for all concerned, friends and family should not try to steer the person away from these issues.
What to do if someone is suicidal
If someone close to you is suicidal or unsafe, try:
- Talking to them about it and encourage them to seek help.
- Remembering that if someone is feeling like their life is not worth living, they are experiencing overwhelming emotional distress.
- Helping the person to develop a safety plan involving trusted close friends or family members that can keep the person safe in times of emergency.
- Removing risks (e.g. take away dangerous weapons or items if that person is angry or out of control and threatening to disappear).
Self care for carers
(A carer is someone who provides support to a friend, family member, or neighbor in need of help because of their age, disability, or physical or mental health.)
- Carers are also likely to experience stress. Depression and hopelessness have a way of affecting the people around them.
- Therapy can release difficult thoughts and emotions in carers too. So, part of caring is for carers to look after themselves to prevent becoming physically run down and to deal with their internal thoughts and emotions.
- Treatment has a positive time as well; when the person starts to re-engage with the good things in life and carers can have their needs met as well.
Key points to remember
- If you are worried that someone is depressed or has bipolar disorder, try talking to them about it in a supportive manner and suggest that they see a mental health professional.
- If they don’t want to seek help, explain the reasons for concern and perhaps provide them with some relevant information.
- Young people are particularly vulnerable to depression.
- Patience, care and encouragement from others are all vital to the person who is depressed.
- If a loved one talks of suicide, encourage them to seek help immediately from a mental health professional.
- Depression can take a toll on carers and close family members – it is important for these people to take care of themselves as well.
Contact Us
Coolminds
Email: hello@coolmindshk.com
Black Dog Institute
Email: blackdog@blackdog.org.au
Where to get more help and support
Bilingual Web Resources
Mind Hong Kong – “Am I A Carer?”
Mind Hong Kong – “What Can Friends and Family Do To Help?”
Student Health Service – “Understanding Depression”
Student Health Service – “Emotional Health”
English-Only Web Resources
Reach Out: a web-based support for adolescents
Headspace online: help for young people
Bilingual Telephone Hotlines
Samaritans Hong Kong 24-hour hotline: 28960000
Samaritan Befrienders Hong Kong 24-hour hotline: 23892222
Suicide Prevention Services 24-hour hotline: 23820000
Suicide Prevention Services “Youth Link” hotline (available 2pm-2am): 2382 0777
Hospital Authority Mental Health 24-hour Hotline: 2466 7350
Social Welfare Department Hotline: 2343 2255
Chinese-Only Telephone Hotlines
Youth Outreach 24-hour hotline service: 90881023
The Hong Kong Federation of Youth Groups “Youthline” hotline (available Mon-Sat, 2pm-2am): 27778899

Resources
Depression in Adolescents & Young People
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to the Black Dog Institute for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to the Black Dog Institute’s website: www.blackdoginstitute.org.au
What this fact sheet covers:
- Signs of depression in adolescence
- Where to get help for an adolescent
- Key points to remember
- Where to get more information
Introduction
- A 2017 study by the Hong Kong Federation of Youth Groups found that of the 3,441 secondary school and university students surveyed, 51% displayed symptoms of depression and close to 40% experienced high levels of stress (7 on a scale of 10).
- According to research done by the University of Hong Kong, more than two-thirds of Hong Kong’s university students experience symptoms of mild to severe depression.
- The HKJC Centre for Suicide Research and Prevention observed that suicide rates for full-time students increased by 76% between 2012 and 2016.
- Onset of depression is typically around mid-to-late adolescence, and it is important to recognise the early warning signs and symptoms. Early intervention can often prevent the development of severe depressive illness.
Developmental Impact
- The teenage years are a time when individuals develop their identity and sense of self.
- If depression is left to develop, it can lead to isolation from family and friends, risk-taking behaviours such as inappropriate sexual involvements and drug and alcohol abuse.
- It can also impact on school performance and study, which can have downstream effects on later career or study options.
- Both biological and developmental factors contribute to depression in adolescence. If bipolar disorder or psychosis is suspected, an assessment by a health professional is recommended. See our Fact Sheet “Symptoms of Bipolar Disorder” for more information.
Signs of depression in an adolescent
- An adolescent who is depressed may not show obvious signs of depression.
- It is often hard to distinguish adolescent turmoil from depressive illness, especially when the young person is forging new roles within the family and struggling with independence, and having to make academic and career decisions.
Signs of a depressed mood include:
- Lowered self-esteem (or self-worth)
- Changes in sleep patterns, that is, insomnia (inability to sleep), hypersomnia (excessive sleep) or broken sleep
- Changes in appetite or weight
- Inability to control emotions such as pessimism, anger, guilt, irritability and anxiety
- Varying emotions throughout the day. For example, feeling worse in the morning and better as the day progresses.
- Reduced capacity to experience pleasure: inability to enjoy what’s happening now, not looking forward to anything with pleasure such as hobbies or activities.
- Reduced pain tolerance: decreased tolerance for minor aches and pains
- Poor concentration and memory
- Reduced motivation to carry out usual tasks
- Lowered energy levels
Where to get help for an adolescent
- If you think someone you are close to might be depressed, you should encourage them to seek advice from a professional. (At school – school counsellor, social worker. Outside school – doctor, counsellor, psychologist)
- The first step is to speak to a professional who can conduct an assessment, provide options and discuss the next steps to take.
- Other initial sources of help are school counsellors and trusted close family members to whom the young person feels comfortable talking.
- If the young person does not want to seek help, it is best to explain your concerns and to provide them with some information to read about depression.
- There are also some excellent websites designed for young people, as well as confidential online and telephone counselling services in both English and Chinese. Please see our list of services at the end of this fact sheet.
- It’s important for young people to know that depression is a common problem and that there are people who can help.
- If there is any mention of suicide this should be taken seriously, and immediate assistance is available by calling 999 or going directly to the nearest hospital.
Key points to remember
- A 2017 study by the Hong Kong Federation of Youth Groups found that of the 3,441 secondary school and university students surveyed, 51% displayed symptoms of depression and close to 40% experienced high levels of stress (7 on a scale of 10).
- Depression in young people is associated with social withdrawal, drops in performance at school, drug or alcohol use and engaging in risky behaviours.
- It can be hard to distinguish depression from adolescent turmoil; if depression is suspected, an assessment should be sought from a doctor or other mental health professional.
- Immediate help should be sought if a young person talks of suicide.
Contact Us
Coolminds
Email: hello@coolmindshk.com
Black Dog Institute
Email: blackdog@blackdog.org.au
Where to get more Information and Support
Mind Hong Kong – “What Is Depression?”
Student Health Service – “Understanding Depression”
Student Health Service – “Emotional Health”
Bilingual Telephone Hotlines
Samaritans Hong Kong 24-hour hotline: 28960000
Samaritan Befrienders Hong Kong 24-hour hotline: 23892222
Suicide Prevention Services 24-hour hotline: 23820000
Suicide Prevention Services “Youth Link” hotline (available 2pm-2am): 2382 0777
Hospital Authority Mental Health Direct hotline: 24667350
Chinese-Only Telephone Hotlines
Youth Outreach 24-hour hotline service: 90881023
The Hong Kong Federation of Youth Groups “Youthline” hotline (available Mon-Sat, 2pm-2am): 27778899

Resources
Causes of Depression
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to the Black Dog Institute for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to the Black Dog Institute’s website: www.blackdoginstitute.org.au
What this fact sheet covers:
- Factors involved in developing depression
- Key points to remember
- Where to get more information
Introduction
Unlike other illnesses or disorders, there is no simple explanation as to what causes depression.
In general, depression can be due to a number of factors including stresses which can range from mild to severe, combined with vulnerability or predisposition to depression that can result from biological, genetic or psychological factors.
Each type of depression is associated with different mixtures of causes. For psychotic or melancholic depression, physical and biological factors are relevant. In contrast, for non-melancholic depression, the role of personality and stressful life events are important.
Genetic factors
There is strong evidence that genetic factors play a significant role in a person’s predisposition towards developing depression, especially melancholic depression, psychotic depression and bipolar disorder. No single gene is likely to be responsible, but rather a combination of genes.
The predisposition to develop depression can be inherited. The genetic risk of developing clinical depression is about 40% if a biological parent has been diagnosed with the illness, with the remaining 60% being due to factors within the individual’s own environment. Depression is unlikely to occur without stressful life events, but the risk of developing depression as a result of such an event is strongly genetically determined.
Biochemical Factors
Our knowledge of the human brain is still fairly limited, therefore we do not really know what actually happens in the brain to cause depression. It is likely that with most instances of clinical depression, neurotransmitter function is disrupted. Neurotransmitters are chemicals that carry signals from one part of the brain to the next. There are many neurotransmitters serving different purposes. However, three important ones that affect a person’s mood are serotonin, noradrenaline and dopamine.
In normal brain function, neurotransmitters interact with a series of nerve cells, with the signal being as strong in the second and subsequent cells as it was in the first. However, in people who are depressed, mood regulating neurotransmitters fail to function normally, so that the signal is either depleted or disrupted before passing to the next nerve cell.
Physical Illness
In a simple sense, physical illness can lead to depression through the lowered mood that we can all experience when we are unwell, in pain or discomfort, confined and less able to do the things we enjoy.
Illness can also change the body’s functioning in a way that leads to depression. Even if the illness isn’t making us feel down we can still suffer from depression. For example:
- It is known that certain cancers can produce a depressive illness – in these cases a person might be quite unaware that they are suffering from depression.
- Compromised immune functioning might play a part in the emergence of depression, although further research is needed to establish this link.
The ageing brain
As we age, our brain’s general functioning can become compromised and this can affect the neurotransmitter pathways which influence mood state. Three reasons for these changes are worth mentioning in relation to depression:
- Late onset depression: Elderly people who develop dementia may also develop a severe depression for the first time; this type of depression is commonly of a psychotic or melancholic type and reflects the disruption of circuits linking certain basal ganglia and frontal regions of the brain.
- These brain changes can reflect an ageing process, particularly in people who are vulnerable to this kind of ‘wear and tear’.
- In others however, high blood pressure or mini-strokes (often unnoticed by the individual and their family) may contribute. Good blood pressure control can reduce the chance of depression in some people.
Gender
Gender is a partial but incomplete explanation of why people may develop depression. Equal numbers of men and women develop melancholic depression. However, studies have shown that there is a much greater likelihood of women developing non-melancholic depression than men. Some of the explanations for this are:
- Women are more likely than men to ‘internalise’ stress, thereby putting them at greater risk of developing depression.
- Women with unsatisfactory marriages or who are caring for a number of young children are also highly over represented among samples of depressed people.
- Hormonal factors commencing in puberty may account for the increased chance in women of developing anxiety (a precursor to depression) or depression.
Stress
It is important to recognise that nearly every individual can be stressed and depressed by certain events. Most people get over the stress or depression within days or weeks while others do not. Ways that stress can lead to depression include the following:
- Past or long-standing stresses can increase the chances of an individual developing depression in later years e.g. growing up in an abusive or uncaring family may increase the risk of developing depression in adult life.
- Events that affect a person’s self-esteem such as the break-up of a close relationship or marriage
- Feelings of ‘shame’ for example, thinking they have not lived up to their own or others’ expectations.
Personality
Our research has shown that people with the following personality types are more at risk of developing depression than others. Those who are high on the first four factors are at distinctly greater risk to depression (especially non-melancholic depression):
- High levels of anxiety, which can be experienced as an internalised ‘anxious worrying’ style or as a more externalised ‘irritability’.
- Shyness expressed as ‘social avoidance’ and/or ‘personal reserve’.
- Self-criticism or low self-worth.
- High interpersonal sensitivity.
- Perfectionism is somewhat protective against the onset of depression but if depression occurs, it can result in longer episodes.
- A ‘self-focused’ style is likely to be at greater risk for brief depressive episodes only
Key points to remember
- There is no single cause for depression; rather it’s a combination of stress and a person’s vulnerability to developing depression.
- The predisposition to developing depression can be inherited.
- Other biological causes for depression can include physical illness, the process of ageing and gender.
- Stress can trigger depression but understanding its particular meaning to the person is important.
- Certain temperament and personality styles pose risks for developing non-melancholic depression.
Contact Us
Coolminds
Email: hello@coolmindshk.com
Black Dog Institute
Email: blackdog@blackdog.org.au
Where to get more information and support
Mind Hong Kong – “What Is Depression?”
Student Health Service – “Understanding Depression”
Student Health Service – “Emotional Health”
Cheer Centre: Interpretation services for Ethnic Minorities for use of public services
Bilingual Telephone Hotlines
Samaritans Hong Kong 24-hour hotline: 28960000
Samaritan Befrienders Hong Kong 24-hour hotline: 23892222
Suicide Prevention Services 24-hour hotline: 23820000
Suicide Prevention Services “Youth Link” hotline (available 2pm-2am): 2382 0777
Hospital Authority Mental Health Direct hotline: 24667350
Chinese-Only Telephone Hotlines
Youth Outreach 24-hour hotline service: 90881023
The Hong Kong Federation of Youth Groups “Youthline” hotline (available Mon-Sat, 2pm-2am): 27778899

Resources
Obsessive Compulsive & Related Disorders + Young People
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to Orygen for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to Orygen’s website: www.orygen.org.au
People use the word ‘obsession’ a lot in everyday conversation, and it can mean different things to different people. In terms of mental health, ‘obsessions’ are recurrent and persistent thoughts, urges, or images that are intrusive and unwanted. Obsessions become a problem when they affect a young person’s behaviour so much that they interfere with everyday life.
Obsessions often go together with compulsions – these are irresistible urges to behave in a certain way. Obsessive– compulsive (OCD) and related disorders are serious, anxiety-related conditions that affect a young person’s everyday life through things like stopping them from getting to school on time, finishing homework, or going out with friends.
What is normal and what is OCD?
Almost everybody experiences the type of thoughts that people with OCD have, such as wanting to double-check they have switched off the oven or double-checking they have locked the front door before they go out. While it’s also very common for people to repeat certain actions, most people can dismiss these thoughts or urges.
People with OCD can’t ignore unpleasant thoughts and pay undue attention to them. This means that the thoughts become more frequent and distressing. Over time, the thoughts can affect all areas of a person’s life, including their school or work activities, their family, and their social life. Young people often develop compulsive behaviours to manage their distress, but these behaviours tend to take up a lot of time – sometimes more than an hour a day.
What are the common obsessive-compulsive and related disorders?
Obsessive–compulsive disorder (OCD)
Young people living with this condition experience repetitive and upsetting thoughts and sometimes compulsive behaviours.
Body dysmorphic disorder (BDD)
A young person living with BDD has an obsession with a perceived defect in their appearance. If other people hardly notice the perceived defect, then the obsession is regarded as markedly excessive. Take a look at the Eating & body image disorders + Young People factsheet to find out more.
People with OCD can’t ignore unpleasant thoughts and pay undue attention to them.
Trichotillomania (compulsive hair pulling) and compulsive skin picking
These are two distinct but related disorders that have obsessive– compulsive features. Young people with these disorders experience a build-up of anxiety that’s relieved by either repetitive hair pulling or skin picking, which are done consciously or unconsciously. Feelings of depression or hopelessness often follow because the young person realises the damage caused by these behaviours. Even if there is no anxiety beforehand, the young person may find pulling or picking pleasurable, and this makes the behaviour difficult to stop.
If these behaviours are because a young person is concerned about their appearance, then the condition may be body dysmorphic disorder.
What are the symptoms of OCD?
Obsessions
Obsessions are unwanted, intrusive, or upsetting thoughts or images that come to mind over and over again. They are difficult to get rid of and can feel silly or unpleasant. Some examples of obsessions include:
- fears about germs and disease
- needing things to be in a certain order
- ‘I must count to twenty or something bad will happen’
- unwanted thoughts about sexual or violent acts.
Compulsions
Compulsions are the actions or rituals that a person carries out in order to get rid of, prevent or ‘neutralise’ the obsessions. People with OCD also carry out compulsions to try to relieve the anxiety caused by the obsessions. Often, people try to stop themselves from doing these things because they realise it’s illogical, but they feel frustrated or worried if they can’t finish them. Some examples of compulsions include:
- washing hands again and again
- repeatedly checking that the light is switched off
- mental rituals, such as counting or repeating words in your head
- hoarding or collecting things that are unnecessary or useless.
OCD and related disorders are treatable, and most young people can learn to stop performing their compulsive rituals and to decrease the intensity of their obsessive thoughts
Other problems
Young people living with OCD or a related disorder may also experience other mental health difficulties, such as depression, other anxiety conditions, an eating disorder, or alcohol and other substance-use problems. Young people with OCD often experience feelings of intense shame about their need to carry out compulsions. These feelings of shame often make the OCD worse. Shame and the consequent secrecy associated with OCD can lead to a delay in diagnosis and treatment. This can lead to long-term health, mental health and relationship problems. Seeking the right support for what’s going on can assist with recovery and planning for getting on with education, work and relationships.
Advice and referral
OCD and related disorders are treatable, and most young people can learn to stop performing their compulsive rituals and to decrease the intensity of their obsessive thoughts.
If you’re having difficulties with OCD
Talk about your concerns with someone you trust, such as a school counsellor, family friend, a parent or teacher. Your GP can help you sort out what is and isn’t OCD, and help with a plan for getting better if you need.
If you think a young person you know is having difficulties
Let them know you’re there to support them, and encourage them to get professional support. Try to avoid giving reassurance to a young person with OCD because as part of their recovery they’ll need to confront their fears without constant reassurance. Don’t involve yourself in the young person’s compulsions – helping them carry out compulsions only makes it more difficult for them to recover. Instead, working with a professional during treatment may give you a role in helping the young person to resist the completion of rituals.
Treatment for OCD and related disorders
OCD and related disorders are usually treated with the help of a professional using cognitive–behavioural therapy (CBT), with exposure and response prevention. CBT is based on the idea that moods and emotions are influenced by thoughts. It explores thinking patterns and how they affect our behaviour and emotions, such as fear.
Exposure and response prevention involves slowly and carefully supporting a young person to confront the feared situations without performing their compulsive behaviours. This helps the young person to learn to tolerate the immediate distress and leads to a reduction in anxiety over time. In certain instances medication may also be helpful.
Getting help
If you, or someone you care about, experiences symptoms of an obsessive– compulsive or related disorder, use these tips to seek help.
- Talk to someone you trust help. Tell family or friends about what you’re feeling and thinking so they can support you.
- Try to eat healthily, get some regular exercise, and find ways to relax by doing things you enjoy (e.g. listening to music, reading a book, or engaging in other hobbies).
- Try to avoid alcohol and other drugs as they often make the anxiety associated with obsessions or compulsions worse over time, and can lead to other problems, such as dependency.
- It can be useful to keep a diary of the frequency, intensity and types of unwelcome thoughts (obsessions). Resist completing rituals (compulsions) as much as possible.
- Do some research to understand your treatment and recovery options – seeking professional help from a counsellor, psychologist, psychiatrist, or a doctor can be helpful.
Exposure and response prevention involves slowly and carefully supporting a young person to confront the feared situations without performing their compulsive behaviours
Further information
For further information regarding mental health, or for information in other languages, visit:
Australia / International
- www.orygen.org.au
- www.headspace.org.au
- www.reachout.com
- www.youthbeyondblue.com
- www.beyondblue.org.au
- www.betterhealth.vic.gov.au
- www.sane.org
- www.healthdirect.gov.au
- www.oyh.org.au
Hong Kong
Disclaimer: This information is not medical advice. It is generic and does not take into account your personal circumstances, physical wellbeing, mental status or mental requirements. Do not use this information to treat or diagnose your own or another person’s medical condition and never ignore medical advice or delay seeking it because of something in this information. Any medical questions should be referred to a qualified healthcare professional. If in doubt, please always seek medical advice.

Resources
Autism Spectrum Disorder (ASD) + Young People
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to Orygen for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to Orygen’s website: www.orygen.org.au
Autism spectrum disorder (ASD) is a developmental condition that can be identified from early childhood onwards and can affect a person throughout their life. The cause is unknown, and there’s no specific medical or genetic test to diagnose it. Instead, diagnosis is based on the presence of: particular patterns of social communication and interaction, restricted interests, and rigid routines, repetitive behaviour (e.g., lining up objects) or repetitive speech.
The diagnosis of ASD has replaced three diagnoses that were previously used: autistic disorder, Asperger’s syndrome and pervasive developmental disorder – not otherwise specified. These disorders no longer exist as separate diagnoses. Instead, they are reflected in the autism spectrum by specifying whether a person has mild, moderate or severe symptoms and difficulties.
With early intervention and support, young people with ASD can begin to understand how their experience of the world is different from others, and can begin to make sense of what supports they might need to live the kind of life that they want.
Areas of difficulty
Social communication and interaction
People with ASD typically have some differences in the way that they communicate and socialise. People with ASD have difficulty understanding the feelings, thoughts and intentions of others and difficulty identifying and communicating their own feelings, thoughts and intentions to others.
While many young people with ASD speak fluently, they might have problems in the area of ‘pragmatic’ language – that is, using language appropriately in social situations. This might mean they find it difficult to hold two-way conversations. A tendency for making literal interpretations can mean figures of speech and sarcasm are misunderstood or misused. Problems with pragmatic language might also lead to people having trouble using the right language for a social situation – their language might be very formal, and their vocabulary might be very rich.
Young people with ASD might also prefer to be alone or seem uninterested in others. Difficulties in reading social cues or situations, expressing empathy and understanding others mean that they might need help to interact with others. They also might have difficulty with eye contact, facial expressions and body language and forming or maintaining social relationships.
Areas of difficulty for young people with ASD
- Social
- Communication
- Behaviour
- Body
- Thinking
With early intervention and support, young people with ASD can begin to understand how their experience of the world is different from others
Interests and behaviours
Young people with ASD often develop special interests that are unusual in their intensity and focus. Public transport, maps, physics and computers are all examples of the wide and varied special interests of people with ASD. Young people with ASD prefer situations to be consistent and may have special preferences with respect to routine and consistency. As a result, young people with ASD might experience difficulties managing change and transition. Activity participation, diet and clothing might be areas in which young people with ASD express unusual rigidity.
Thinking
Young people with ASD are often logical thinkers and can be good with facts, figures and details. This logical thinking may mean that they can have difficulty understanding non-concrete ideas.
ASD and the body
Young people with ASD might experience clumsiness and problems with body awareness that can lead to difficulties with sports, handwriting and other physical skills. Young people with ASD frequently have problems with sleep and can be very sensitive to different sensations – finding a particular noise disturbing, or a particular item of clothing very uncomfortable.
Young people with ASD often develop special interests that are unusual in their intensity and focus
What might not be so bad about it?
Whilst people with ASD might have difficulties in a range of areas, they might also present with admirable differences in perception, attention, memory and intelligence.
ASD, youth and mental illness
Youth is a tricky time. For young people with ASD, things like progressively more complex social demands, increasingly difficult skills to be learned at school or home and transitions, such as graduating, might all be stressful. It’s often at this time that young people with ASD and others around them might become more alert to their social differences. Young people with ASD might feel excluded, bullied and frustrated by their differences. These negative experiences can leave young people with ASD at risk of low self-esteem and at increased risk of developing mental ill-health, such as depression and anxiety.
When young people with ASD develop mental illness, diagnosis and treatment need to be tailored to account for the young person’s different personality style and their differences in the areas of socialising, communication and interests.
For some young people, it’s only during their treatment for mental health difficulties that they or their family may raise suspicions about ASD. Diagnosis of ASD is a reasonably lengthy process involving multiple health professionals. Diagnosis is important for young people because it provides effective treatment options and helps to better address their needs.
Treatment
Effective treatment will target any mental health difficulty, support the young person to adjust to the changes they have as a result of ASD and make use of the skills that they have. Many people with ASD might still find social situations, personal relationships and major life changes challenging, but with support and encouragement, many people go on to undertake further education, develop their interests through hobbies and membership of clubs, work successfully in jobs that interest them and find fulfilling friendships.
Young people with ASD are often logical thinkers and can be good with facts, figures and details
Supporting someone who lives with ASD
Here are some ways you can help someone you know who lives with ASD.
- Any approach to support someone with ASD needs to be unique and individualised.
- Encourage the person to talk about what’s going on for them, and any troubles or worries they have. It might be hard for them to find the right words or to express themselves, so be patient and try other preferred routes for communication (e.g. stories/drawings).
- Help them build confidence through doing things that use their strengths.
- Some people with ASD can find being around other young people who feel ‘different’ supportive. Groups at schools, local councils and health services might be options, and internet forums and chat rooms can also be helpful and accessible.
- Have a routine and try to be consistent. It doesn’t need to be too rigid, but might mean that a young person with ASD can begin to take advantage of planned opportunities to talk to you about their worries or hopes.
- Be patient. It takes a lot longer for people with ASD to get used to things and make changes in their lives.
Further information
For further information regarding mental health, or for information in other languages, visit:
Australia / International
Hong Kong
- Child Assessment Service, Dept. of Health, HK (Government)
- Early Education Training Centre
- Autism Partnership
- The Rainbow Project
- Autism Recovery
- Autism Children’s Foundation
- The Hong Kong Down Syndrome Association (Chinese)
- Society for the Welfare of Austistic persons (Chinese)
- AnAn International Education Foundation Hong Kong
- SAHK: Support Service for Persons with Autism Spectrum
- List of assessment service providers (Chinese)
Disclaimer: This information is not medical advice. It is generic and does not take into account your personal circumstances, physical wellbeing, mental status or mental requirements. Do not use this information to treat or diagnose your own or another person’s medical condition and never ignore medical advice or delay seeking it because of something in this information. Any medical questions should be referred to a qualified healthcare professional. If in doubt, please always seek medical advice.

Resources
Eating & Body Image Disorders + Young People
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to Orygen for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to Orygen’s website: www.orygen.org.au
Eating disorders and body image disorders are serious mental illnesses in which eating, weight or dissatisfaction with one’s appearance becomes an unhealthy preoccupation in a person’s life. Adolescence is the peak period for onset of these disorders and they lead to significant interference with day to day life.
Eating and body image disorders can occur when the expectations of how a young person wants their body to look doesn’t match up to reality. Negative thoughts about body image and self-worth can lead to changes in eating and exercise behaviours or compulsive behaviours, which at their worst can be life threatening. Both males and females can become excessively concerned with body image, size, weight, fitness, shape and perceived defects, and as a result of this preoccupation, change their behaviour in unhealthy ways.
Types of eating and body image disorders
Anorexia Nervosa
Anorexia Nervosa is characterised by the restriction of energy intake (reluctance or refusal to eat) leading to significantly low body weight, intense fears and thoughts about body size (worry about becoming fat), and distorted perceptions of body weight (denial that weight is too low).
Bulimia Nervosa
Bulimia Nervosa is characterised by recurrent episodes of binge eating (overeating with a sense of no control) followed by compensatory behaviour, like self-induced vomiting (purging), misuse of laxatives, fasting or excessive exercise.
Binge Eating Disorder
Binge Eating Disorder is characterised by recurrent and rapid episodes of binge eating (overeating when not physically hungry combined with a sense of no control over what or how much is eaten). The type of food eaten can vary, but often eating occurs alone and is followed by feelings of shame, depression and guilt. The young person usually eats food quickly until they become uncomfortably full, and then will become emotionally distressed, embarrassed and fatigued.
Other Specified Feeding or Eating Disorder
An Other Specified Feeding and Eating Disorder is characterised by many of the symptoms of another eating disorder – such as Anorexia Nervosa, Bulimia Nervosa or Binge Eating Disorder – but the full criteria for diagnosis of one of those disorders isn’t quite met. This category includes Atypical Anorexia Nervosa, where weight is within or above the normal range, and Purging Disorder, which is engaging in a recurrent behaviour to influence weight or shape in the absence of binge eating.
Body Dysmorphic Disorder
Body Dysmorphic Disorder is characterised by a preoccupation (obsession) with a perceived defect in a person’s appearance. This causes significant distress or disruption in social, school or occupational life. If a slight defect is present, which others hardly notice, then the concern is regarded as markedly excessive. These obsessions are hard to resist or control and make it difficult to focus on anything but the imperfections. This can lead to low self-esteem, avoidance of social situations, and problems at work or school. Often some type of compulsive or repetitive behaviour is performed to try to hide or improve the flaws, although these behaviours usually give only temporary relief.
Other difficulties
Young people with an eating or body image disorder may also experience other mental health difficulties, including depression, anxiety or substance use. A young person with an eating or body image disorder may go to great lengths to hide, disguise or deny their behaviour, or do not recognise that there is anything wrong. This can result in a delay in getting treatment, which means that long-term health, mental health and relationship problems are more likely. Getting the right support for what’s going on now can assist with recovery and planning for getting on with education, work and relationships.
Medical teams should be involved in the treatment of eating and body image disorders because all these disorders can lead to serious physical health issues, psychological distress and emotional and relationship problems. Starvation, repeated cycles of binge-eating and purging or fasting can lead to major metabolic and other chemical changes in the body as well as damage to vital organs. If a young person has extreme weight loss, as is the case with Anorexia Nervosa, they may need to be kept safe while they restore their weight.
It’s in these cases that assessment and treatment should use a medical or a specialised team approach.
A young person with an eating or body image disorder may go to great lengths to hide, disguise or deny their behaviour, or do not recognise that there is anything wrong
Advice and referral
Talk about your concerns and difficulties. You might choose to talk with someone you trust, such as a school counsellor, family friend, a parent, teacher or other support. Your GP can help to sort out what is and isn’t an eating or body image disorder and help with a plan for getting better.
If someone you know has an eating or body image disorder, let them know you’re there to support them and, if needed, encourage them to get professional support.
There are effective treatments to help young people who experience eating and body image disorders. The type of treatment will depend on the type of disorder. One of the most commonly used treatments is cognitive behaviour therapy (CBT). CBT explores thinking patterns and how they affect our behaviour and emotions. There are other psychological treatments for eating and body image disorders, including family approaches for when adolescents or young people are experiencing an eating disorder. In certain instances medication may also be helpful. If a young person does need medical treatment, there are health professionals and treatment programs that specialise in eating disorders.
If someone you know has an eating or body image disorder, let them know you’re there to support them
Ask family and friends to support you to eat in a healthy and balanced way
Getting help
If you or someone you know experience symptoms of an eating or body image disorder, you can use these tips to start seeking help.
- Talking to someone you trust helps. Tell family or friends about what you’re feeling and thinking so they can support you.
- Ask family and friends to support you to eat in a healthy and balanced way.
- Try to find ways to relax by doing things you enjoy (e.g. listening to music or reading or other hobbies).
- Try to avoid alcohol and drugs as they often make the situation worse over time, and can lead to other problems (e.g. dependency).
- Do some research to understand your treatment and recovery options. It may be useful to seek professional help from a counsellor, psychologist, psychiatrist or doctor.
Further information
For further information regarding mental health, or for information in other languages, visit:
Australia / International
- www.orygen.org.au
- www.headspace.org.au
- www.reachout.com
- www.youthbeyondblue.com
- www.beyondblue.org.au
- www.betterhealth.vic.gov.au
- www.sane.org
- www.healthdirect.gov.au
- www.eatingdisorders.org.au
- www.nedc.com.au
- www.oyh.org.au
Hong Kong
Disclaimer: This information is not medical advice. It is generic and does not take into account your personal circumstances, physical wellbeing, mental status or mental requirements. Do not use this information to treat or diagnose your own or another person’s medical condition and never ignore medical advice or delay seeking it because of something in this information. Any medical questions should be referred to a qualified healthcare professional. If in doubt, please always seek medical advice.

Resources
Mental Health Problems in Children and Young People: Guidance for Parents and Carers
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
We would like to acknowledge the Charlie Waller Memorial Trust (CWMT) UK for these resources and for allowing us to adapt this. For the original version of this resource, please refer to the CWMT website: www.cwmt.org.uk
Looking after a child or young person who has emotional or mental health problems can be very hard. You may feel challenged, isolated, scared and deeply upset and wish you knew where to turn for help.
What is this leaflet for?
This leaflet offers guidance on how best to support your child and where to find further advice and help with their mental health.
Be assured, things can improve for your child. Mental health, like physical health, is relevant to all of us, including children and young people. Problems are often temporary and, with support, can change for the better.
Seeking help
You are not alone. Many parents and carers have similar concerns and stresses, although they may not feel able to discuss them openly. There is good support and guidance, through national and local organisations. On the back of this leaflet is a list of reliable organisations that offer information based on sound evidence. Do have a look to find out which sources of support might be best for you.
The sooner you seek help, the better. Every local area is different but the three places listed below are a good place to start.
Talk to your GP
Your GP will listen, begin to understand your child’s needs and suggest the most appropriate course of action or support for your child, including referral to mental health specialists, if necessary.
So, make an appointment for your child and explain your concerns when you do so. You might also find it helpful to make a second appointment with the GP, for yourself, to discuss the “ripple effects” of your child’s difficulties on the rest of the family.
“[I spoke] about my hopelessness and sadness to a teacher, who called my Mum, and arranged for us to see my GP. A year later, I have just turned 16 and am in a completely different place to where I was a year ago.”
Help at school
School is an important part of the picture when it comes to children’s mental health. It’s a good idea to stay in communication with the school about the issues your child is experiencing. There may well be sources of help and support within the school, so do encourage your child to talk to a trusted teacher or member of support staff.
“The younger generation will hopefully grow up where mental health is not something that is ignored but something that should have everyone’s attention.” Teacher
Integrated Family Service Centre
Funded by the Social Welfare Department, IFSC’s are located all across Hong Kong. You can approach to receive support for your child, young person of family. Their social workers can provide counselling services or refer you out to a psychologist if necessary. You can call 23432555 to locate the IFSC for your family.
What you can do to help your child
As a parent you can have a crucial role in your child’s recovery. The more you can understand about mental health and your child’s difficulties, the more confident you will be in supporting them. Getting professional help can be important but there is a great deal you can do as a parent too. Every case is individual, but these general tips might help you to help your child:
Encourage them to talk
Try ‘open-ended’ questions like, “How are things for you?” “What’s happening with you?” “What do you think or feel about…?” or “What’s on your mind?”, rather than questions that have “yes/no” answers.
When discussing their problem, don’t try to ‘fix’ it. For the most part, young people simply need to know you are there to support them.
Listen and be understanding
Listen calmly and try not to judge your child. Let them know you are happy to listen while they chat about anything and everything, whenever they want to. Never underestimate the importance of being an attentive, non-judgmental listener.
Remember, you don’t need to know all the answers, listening without responding is often enough.
Give your child reliable self-help information from trusted sources, based on sound evidence
They can read and use this at their own pace, allowing them some privacy, but at the same time you are showing you are there to help and they are not alone. Peer-to-peer support can be really useful. Self-help links include:
- HKUST Counseling and Wellness Center Publications (Hong Kong)
- HKU CEDARS Mental Health & Enrichment Information (Hong Kong)
- epicfriends.co.uk (UK)
- studentsagainstdepression.org (UK)
Tell them, and show them, how much you care and how important they are in the family
It is not easy when stress levels are high, but a peaceful, loving home life can really help recovery. Keep family routines as normal as possible and do simple things together – maybe watching a film, or having a meal, going for a walk or playing a game. Just doing simple everyday things together (like grocery shopping or cooking) can provide a really helpful distraction. This can bring everyone in the family closer.
Enjoy the time you spend together but understand that it might be a while before your child starts enjoying activities again. Try not to pressurise them and, if they need a little space, support them with that while not leaving them isolated.
Understand the problems
As with physical health, there are many different ways of experiencing mental health issues. Try to read up on your child’s specific problems. This will help you understand their experiences and what helps recovery, building their confidence for the future.
Encourage social contact with friends and family
Encourage your child to go out (if only for short periods) and to keep in touch with friends.
Simple physical activity
Taking regular exercise, such as going for walks, can help improve mood and reduce anxiety.
Know that recovery will not happen overnight
As a parent or carer, you want to make your child feel better immediately but, like physical health problems, mental health problems can sometimes take time to improve and some, such as eating disorders, may be complex and seem illogical. There will often be ups and downs in recovery.
Don’t be afraid to seek further advice from mental health professionals
Many of them have a great deal of experience and are generally an excellent source of guidance and support.
Don’t blame yourself
Parents or carers often feel guilty, thinking they have caused the problems, perhaps through genetics or the home life they have created. Usually, this is not the case.
Look after yourself
In order to support your child, you need to stay strong and well yourself. Often it helps to talk to someone, so don’t be scared about doing this, with friends, family or a parent helpline. For further resources and support for parents please visit the online helplines and resources on www.coolmindshk.com
Hong Kong organisations which help parents
Mind Hong Kong provides information and advice on a range of mental health topics, as well as a community directory of available resources.
New Life Psychiatric Rehabilitation Association provides a Family Support Service. They aim to build a holistic support network among carers to support them to face challenges with a positive mindset and to maintain family functions.
Caritas Family Crisis Support Center (in Chinese only) aims to manage family crisis at an early stage by providing integrated and easily accessible services to assist individuals or families in crisis or distress. Services provided include 24-hour hotline service (18288) and short-term emergency accommodation.
Youth Outreach (in Chinese only) has a 24-hour hotline for young people from ages 8 to 18. The organisation also provides support through emergency accommodation, individual and family counselling, academic and career advice, among others.
Hong Kong Eating Disorders Association
In addition to patient support groups and members gatherings, they host small
group gatherings for caregivers to share and de-stress.
Baptist Oi Kwan Social Service has a family resource and service centre providing support and counselling for families of those recovering from mental illnesses.
Christian Family Service Centre provides education, counselling, groups, shelter and other services to children and families. They aim to help overcome family problems, provide quality learning environment, and build up their mutual support networks.
International organisations which help parents
Young Minds is an excellent source of information about all aspects of child mental health, including a Parent Helpline.
Minded for Families provides free, quality- assured advice which is easy to understand. It is helpful for any adults caring for children or teenagers with mental health problems.
Beat gives clear advice on all aspects of dealing with eating disorders, including helpful guidance to parents, carers and families.
Anna Freud Centre – a leaflet about mental health for parents of young children.