Resource Topics: supporting others/yourself


Resources
MythBuster – Trauma and mental health in young people: Let’s get the facts straight
Introduction
Most young people will have been exposed to at least one traumatic event in their lifetime. Multiple and prolonged exposure to trauma is also common. When a young person reaches out to open up about trauma, the way that others around them respond can have a massive impact on the young person’s ability to understand and cope with their experiences. Yet some aspects of trauma remain largely misunderstood, particularly its relationship with mental health.
This mythbuster has been created for young people, their families, and carers to replace some of the most common and harmful myths about trauma in the mental health space with a better understanding of what trauma is and how it can affect young people.
Trauma can come from many different life experiences
What is trauma?
Trauma is broadly described as a deeply distressing experience that can be emotionally, mentally, or physically overwhelming for a person. It takes on many different forms and effects vary from one person to another (van der Kolk et al., 2005; Bryson et al., 2017). It is important to know that an experience does not have to be life threatening to be traumatic. Approximately two thirds of young people will have been exposed to a traumatic event by the time they turn 16 (Copeland et al., 2007). Experiencing a traumatic event can potentially affect both their current and future mental health.
What types of events cause trauma?
Trauma can arise from many different life experiences. Some examples of different types of trauma are listed below:
Direct and indirect trauma
Some types of trauma are called ‘direct trauma’, and others are called ‘indirect trauma’ (May & Wisco, 2016). A ‘direct trauma’ is experienced first-hand or by witnessing a trauma occurring to another person. An ‘indirect trauma’ comes from hearing or learning about another person’s trauma second-hand.
Single event trauma
Single event trauma is related to a single, unexpected event, such as a physical or sexual assault, a fire, an accident, or a serious illness or injury. Experiences of loss can also be traumatic, for example, the death of a loved one, a miscarriage, or a suicide.
Complex trauma
Complex trauma is related to prolonged or ongoing traumatic events, usually connected to personal relationships, such as domestic violence, bullying, childhood neglect, witnessing trauma, emotional abuse, sexual abuse, or torture.
Vicarious trauma
Vicarious trauma can arise after hearing first-hand about another person’s traumatic experiences. It is most common in people working with traumatised people, such as nurses or counsellors. Young people may also experience vicarious trauma through supporting a loved one who is traumatised (e.g. a parent or a friend).
Trans- or intergenerational trauma
Trans- or intergenerational trauma comes from cumulative traumatic experiences inflicted on a group of people, which remain unhealed, and affect the following generations (Hudson, Adams & Lauderdale, 2016). It is most common in young people from refugee or migrant families.
Anyone can experience trauma, regardless of their age or social/cultural background
Who experiences trauma?
Some young people are at higher risk of being victimised, abused, marginalised, excluded, and/or experiencing unsafe situations that leave them vulnerable to potentially traumatic experiences. Young people who are more likely to have experienced trauma include those in out-of-home care, in the juvenile justice system, those experiencing homelessness, young refugees or asylum seekers, and young people working in emergency services (Orygen, 2017). However, it is very important to understand that anyone can experience trauma, regardless of their age or social/cultural background.
How do our perceptions of traumatic events change as we age?
When trying to understand the impact trauma has on the lives of young people, it is important to understand the way we make sense of and respond to trauma as we age. During childhood we are more sensitive to our environment, so how we view threats can be quite different to the way adults view threats (Odgers & Jaffee, 2013). For example, during COVID, parents may be distressed about the safety of their children, the loss of their livelihood, and the impact on their community. On the other hand, children may be most distressed about separation from their extended family and school friends, and the disruption of their daily routines (The Australian Child and Adolescent Trauma Loss and Grief Network, 2010). This can mean that adults might be confused or unable to relate to their child’s response to a traumatic event. Likewise, a child may also be confused by their parents’ reactions and/ or why they might not be feeling or responding to an event in the same way.
Young people and children process trauma differently
As their brains are still developing, children process trauma differently compared to adults. This means that the types of things that children interpret as traumatic, and how they understand them, can be very different to adults.
When looking back at traumatic experiences in childhood, it can be hard to understand the confusing emotions and reactions experienced at the time. A young person might look back and think that they should have been able to understand things ‘better’ or cope ‘better’. This can lead to strong and difficult feelings like anger, guilt, and shame.
When a young person is caught up in this way of thinking, they may cope with an ‘adult’ response. In other words, they attempt to look back on their experiences in childhood through the lens of an adult. By doing this, it is easy to forget that the trauma happened to a child, who has much less ability and life experience, to help them process their trauma and seek support.
The way we make sense of and respond to trauma changes as we age
How does trauma affect young people?
Short-term effects
The short-term effects of trauma are often described as normal reactions to abnormal events (Jones & Wessely, 2007), and can include:
- fear
- guilt
- anger
- isolation
- helplessness
- disbelief
- emotional numbness
- sadness, confusion
- flashbacks or persistent memories and thoughts about the event (van der Kolk, 2000)
It is really important to know that these are normal and healthy reactions to trauma. These can last for up to a month after the trauma has occurred, and can slowly reduce over time.
Long-term effects
Sometimes these strong emotions, thoughts, and memories can continue and even worsen over time. This can overwhelm a young person and have damaging effects on their life and course (e.g. their wellbeing, relationships, and their ability to work and/or study) (Orygen, 2017). Some traumas, such as those occurring in childhood, may have effects that only become clear later in life (Felitti, 2002). In the long-term, there is a strong relationship between trauma and poor mental and/or physical health outcomes; however, in many cases young people can bounce back with the right support (Iacoviello & Charney, 2014; Felitti et al., 1998). Additionally, in some situations, young people can draw personal strength from their struggle with trauma and experience a feeling of positive growth (Meyerson et al., 2011).
Developmental effects
Being exposed to trauma when individuals are very young can change how their brain grows and negatively affect their ability to learn (Whittle et al., 2013; Malarbi er al., 2017). Experiencing high levels of stress at a young age can also increase risk-taking behaviours in adolescence and early adulthood, which can lead to poor physical health later in life (Felitti, 2002).
What is post-traumatic stress disorder or PTSD?
Post-traumatic stress disorder (PTSD) is the most commonly talked about trauma-related diagnosis. Symptoms include having intrusive memories of the traumatic event, increased stress, avoidance of situations and/or people associated with the trauma, and increased negative thoughts (American Psychiatric Society, 2013). These symptoms impact a person’s ability to keep up with their day-to-day life and make it hard for them to focus on work and/or study and other tasks.
In Hong Kong, an increase of people experiencing PTSD symptoms has risen to approximately more than 30% in 2019. PTSD can also cause problems with a person’s relationships with others (Koenen et al., 2017), and symptoms may differ between children, adolescents, and adults (Mikolajewski, Scheeringa & Weems, 2017). Thus, it is really important to get help early if you are struggling to cope after experiencing trauma because evidence shows that the sooner help is sought, the lower the risk of developing PTSD (Gillies et al., 2016).
Evidence shows that the sooner help is sought, the lower the risk of developing PTSD
What are the most common myths about trauma?
Traumatic events and a young person’s reaction to them vary a lot. They can vary between people (e.g. some people may be more sensitive to traumatic experiences than others), within the same person over time, or differ depending on the type of traumatic event the person has experienced.
This can make it difficult for us to have a shared understanding of what trauma is and how it can affect people. If we feel confused or uncertain about what trauma is and how it can affect someone, it would be very easy to end up believing in common and unhelpful myths instead.
Below are some of the common myths surrounding trauma and the reasons why these myths are harmful and untrue.
MYTH: “Everyone who has mental ill-health has experienced trauma”
This myth is particularly harmful because young people who have not experienced trauma, but who are struggling with their mental health may feel that they have no right to feel how they do, or become very confused about how they are interpreting their experiences. They may also worry that if they seek support, everyone would automatically assume they have experienced a type of trauma.
Just because a young person is experiencing mental ill-health, this does not necessarily mean that they have gone through trauma. There are many risk factors that contribute to the beginning of mental ill-health. These can be environmental, genetic, social, and cultural in nature (Kieling et al., 2011).
Mental ill-health can start without a specific event ‘tipping a person over the edge’. In fact, mental ill-health is often triggered by a build-up of a number of smaller stressful events rather than one big traumatic event (Fox & Hawton, 2004). Even though trauma is linked to a higher chance of poor mental health, it is important to remember that the causes of mental ill-health in young people are very complex and differ from person to person (Guina et al., 2017; Paus, Keshavan & Giedd, 2008).
It is really important to know that developing mental health problems after trauma is not a sign of weakness
MYTH: “Everyone who has experienced trauma will develop mental ill-health”
Most people who experience trauma do not develop mental ill-health as a consequence (Sayed, Iacoviello & Charney, 2015). Many factors influence whether or not a young person develops mental ill-health after experiencing trauma. These include the severity and type of trauma, the support available, how easily they can access this support, past traumatic experiences, family history, and physical health (Iacoviello & Charney, 2014; Sayed, Iacoviello & Charney, 2015; Brewin, Andrews & Valentine, 2000).
It is completely normal to experience strong or overwhelming emotions after a traumatic experience, but it is when these symptoms last a long time, worsen overtime, or cause other problems (e.g. using substances to cope) that mental health difficulties are likely to arise. It is really important to know that developing mental health problems after trauma is not a sign of weakness, nor does it reflect anything about you personally. It is simply a sign that you may need some extra support to recover from the effects of your experiences.
MYTH: “It’s my fault”
Trauma can happen to anyone, and if you are a victim of trauma, this does not mean that you are to blame for what happened to you. ‘It’s my fault’ is a common thought after experiencing trauma, and it is completely normal to feel shame, guilt, and/or self-blame after these experiences. Even though you may feel this way, it does not mean you deserve these feelings, and a huge part of recovery is working to overcome them.
These types of emotions are particularly common in young people who have been traumatised by another person (e.g. through sexual abuse, physical abuse, bullying, or violent crime). In cases of trauma resulting from abuse, it is important to understand that abuse comes from the needs and motivations of the perpetrator, not the individual. Being able to work through these strong emotions of self-blame, guilt, and/or shame is essential to recovery. This means it is very important to find the right help to support you through this process.
Traumatic events are sometimes singular and life threatening, but many are more complex.
MYTH: “Only bad things come out of traumatic experiences”
Struggling through traumatic experiences often changes the way a person views the world and people around them. A lot of the time, the changes in thoughts are negative (e.g. the world seems scarier, or people seem less trustworthy). However, in some situations, with the right support, and time to heal, a person may also draw strength and positive change from surviving a traumatic event.
When this happens, it is described as ‘post-traumatic growth’ (Linley & Joseph, 2004; Clay, Knibbs & Joseph, 2009; Tedeschi & Calhoun, 2004). When someone experiences post-traumatic growth, they may gain a greater appreciation for life, a feeling of greater personal strength, a deeper connection to others, and even gain new ideas about the path they see their life taking in the future (Tedeschi & Calhoun, 2004). Research shows that post-traumatic growth is hugely influenced by many psychological, social, and environmental factors in a young person’s life (Meyerson et al., 2011). How each of us reacts to traumatic experiences is deeply linked to these factors, and our different reactions do not make us ‘weaker’ or ‘stronger’ compared to others.
MYTH: “Your life must be threatened for an event to be traumatic”
Traumatic experiences take many different forms (Weiss & Gutman, 2017). There does not have to be one defining event that makes something traumatic. It is true that traumatic events are sometimes singular and life threatening, but others are more complex. Many people experience trauma through ongoing or prolonged exposure to events such as abuse, neglect, and bullying. Others may experience trauma vicariously through encountering another person’s traumatic experiences first-hand.
MYTH: “PTSD is the most common response to trauma”
Although post-traumatic stress disorder (PTSD) is the most commonly talked about trauma-related mental illness, it is not the most common mental health diagnosis among people who have experienced trauma. There are many ways that trauma can affect mental health in young people (Sayed, Iacoviello & Charney, 2015). In fact, for most young people, PTSD only captures a small aspect of their mental health state after trauma (van der Kolk & Courtois, 2005). Young people who have experienced trauma can develop a wide range of mental health problems, without developing PTSD (Odgers & Jaffee, 2013). These can include depression (Widon, Du Mont & Czaja, 2007), anxiety (Fernandes & Osorio, 2015), complex PTSD (Resick et al., 2012), borderline personality disorder (Ball & Links, 2009), substance abuse disorders (Stevens, Murphy & McKnight, 2003), eating disorders (Pignatelli et al., 2017), psychosis (Bendall et al., 2008), and suicide-related behaviours (Miller et al., 2013).
Take home messages
- If you have experienced trauma, you are not alone. Trauma in young people is very common and it is important for family, friends, and mental health professionals to be aware of this.
- Traumatic events can be one off (e.g. car accident, sexual assault), ongoing/prolonged (e.g. childhood sexual abuse, bullying, emotional or physical abuse), or experienced second-hand (e.g. witnessing family violence). Any type of trauma has the potential to be very damaging to a young person’s mental health.
- Often young people who have been abused or neglected feel at blame for what has happened to them – they may feel it was their fault, or that they ‘brought it on’ or ‘asked for it’. If you are in this situation, it is very important to know that you are not to blame, no matter how strong the feelings of guilt or shame may be.
- There is no one uniform or ‘right’ way to respond to a traumatic event. Responses to trauma are highly variable. Different people may react very differently, even to the same situation.
- Young people experiencing mental ill-health have not necessarily experienced trauma, and this does not make their mental health difficulties any less ‘real’ or ‘legitimate’.
- Trauma does not always lead to mental ill-health in young people. Many young people exposed to trauma will make a full recovery without needing mental health intervention.
- Experiencing mental health difficulties related to trauma is not a sign of weakness or failure.
- Trauma can lead to a wide range of mental health difficulties, not just PTSD. These can include anxiety, depression, substance abuse, borderline personality disorder, and eating disorders. It is important to get support from a health professional for any of these difficulties.
- It is possible to recover from mental health difficulties related to trauma.
Help is at hand
Support is a huge protective factor against ongoing mental health difficulties related to trauma. Sometimes people can try to cope with the effects of trauma alone, even though reaching out for support can be hugely beneficial. Some young people might feel an overwhelming sense of self-blame or shame and might not be aware of or understand the effects of trauma, making it even harder to seek support.
Seeking help from someone you know
It is really important to try to find someone you can talk to about what’s going on for you. Seeking support for trauma recovery does not make a person ‘weak’, in fact it is a brave step to take on the road to recovery. Opening up about traumatic events can be daunting, making it very important to find someone you feel comfortable with and can trust to talk to. This person could be a family member, friend, or school counsellor.
Seeking professional help
Some young people may not feel comfortable opening up to people in their personal lives and may prefer to seek help through a mental healthcare professional. In terms of seeking professional help, a good place to start is with your doctor, a counsellor, or through a visit to your closest local support group.
A number of helplines in Hong Kong can be found here:
- Emergency hotline: 999
- The Samaritans 24-hour hotline (Multilingual): (852) 2896 0000
- Samaritan Befrienders Hong Kong 24-hour hotline (Cantonese only): (852) 2389 2222
- Suicide Prevention Services 24-hour hotline (Cantonese only): (852) 2382 0000
- OpenUp 24/7 online emotional support service (English/Chinese): www.openup.hk
More hotlines and resources can also be found here:
Want to know more?
Some helpful resources about trauma and its effects include:
- Asking for Help: When it’s time to talk about your mental health- Coolminds and Charlie Waller Memorial Trust (CWMT) UK factsheet
- Seeking help and what to expect- Coolminds factsheet
- Discrimination and Mental Health: A Guide for Young People- Coolminds factsheet
- Voices of Youth: Stigma, Discrimination and Mental Health- Coolminds factsheet
Supporting someone who has experienced trauma can be emotionally overwhelming, making it equally important to look after yourself. If you are concerned about the wellbeing of someone close to you, it is important to reach out for additional help.
Some highly recommended websites that offer more information on how to support to someone affected by trauma include:
- Samaritans Hong Kong
- Samaritans Befrienders Hong Kong
- The Zubin Foundation- Ethnic Minority Well-being Centre (EMWC)
- Christian Action (Woo Sung Centre)
- Yang Memorial Methodist Social Service- Yau Tsim Mong Family Education and Support Centre
- The Salvation Army Youth, Family and Community Services
- Post Traumatic Stress Disorder – Institute of Mental Health Castle Peak Hospital
- BGCA – What is Trauma?
References
1. van der Kolk, BA, et al. 2005, ‘Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma’, Journal of Traumatic Stress, vol. 18, no. 5. pp. 389–399.
2. Bryson, SA, et al. 2017, ‘What are effective strategies for implementing trauma-informed care in youth inpatient psychiatric and residential treatment settings? A realist systematic review’, International Journal of Mental Health Systems, vol. 11, pp. 36.
3. Copeland, WE, et al. 2007, ‘Traumatic events and posttraumatic stress in childhood’, Archives of General Psychiatry, vol. 64, no. 5, pp. 577–584.
4. Hudson, CC, Adams, S & Lauderdale, J 2016, ‘Cultural expressions of intergenerational trauma and mental health nursing implications for US healthcare delivery following refugee resettlement: an integrative review of the literature’, Journal of Transcultural Nursing, vol. 27, no. 3, pp. 286–301.
5. May, CL & Wisco BE 2016, ‘Defining trauma: how level of exposure and proximity affect risk for posttraumatic stress disorder’, Psychological Trauma, vol. 8, no. 2, pp. 233–40.
6. Orygen The National Centre of Excellence for Youth Mental Health, Youth Mental Health Policy Briefing: Trauma and Youth Mental Health. 2017, Orygen: Melbourne.
7. Odgers, CL & Jaffee SR 2013, ‘Routine versus catastrophic influences on the developing child’, Annual Review of Public Health, vol. 34, no. 1. pp. 29–48.
8. The Australian Child and Adolescent Trauma Loss and Grief Network 2010, ‘How children and young people experience and react to traumatic events’, Australian National University, Canberra.
9. Jones, E & Wessely S 2007, ‘A paradigm shift in the conceptualization of psychological trauma in the 20th century’, Journal of Anxiety Disorders, vol. 21, no. 2, pp. 164–175.
10. van der Kolk, B 2000, ‘Posttraumatic stress disorder and the nature of trauma’, Dialogues in Clinical Neuroscience, vol. 2, no. 1, pp. 7–22.
11. Felitti, VJ 2002, ‘The relationship of adverse childhood experiences to adult health: Turning gold into lead’, Zeitschrift Fur Psychosomatische Medizin Und Psychotherapie, vol. 48, no. 4, pp. 359–369.
12. Iacoviello, BM & Charney DS 2014, ‘Psychosocial facets of resilience: implications for preventing posttrauma psychopathology, treating trauma survivors, and enhancing community resilience’, European Journal of Psychotraumatology, vol. 5.
13. Felitti, VJ, et al. 1998, ‘Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study’, American Journal of Preventive Medicine, vol. 14, no. 4, pp. 245–258.
14. Meyerson, DA, et al. 2011, ‘Posttraumatic growth among children and adolescents: a systematic review’, Clinical Psychology Review, vol. 31, no. 6, pp. 949–964.
15. Whittle, S, et al. 2013, ‘Childhood maltreatment and psychopathology affect brain development during adolescence’, Journal of the American Academy of Child and Adolescent Psychiatry, vol. 52, no. 9, pp. 940–952.
16. Malarbi, S, et al. 2017, ‘Neuropsychological functioning of childhood trauma and posttraumatic stress disorder: a meta-analysis’, Neuroscience & Biobehavioral Reviews, vol. 72, pp. 68–86.
17. American Psychiatric Society 2013, Diagnostic and Statistical Manual of Mental Disorders, 5th edn, American Psychiatric Publishing, Arlington.
18. Koenen, KC, et al. 2017, ‘Posttraumatic stress disorder in the world mental health Surveys’, Psychological Medicine, vol. 47, no. 13, pp. 2260–2274.
19. Mikolajewski, AJ, Scheeringa, MS & Weems, CF 2017, ‘Evaluating diagnostic and statistical manual of mental disorders, fifth edition, posttraumatic stress disorder diagnostic criteria in older children and adolescents,’ Journal of Child and Adolescent Psychopharmacology, vol. 27, no. 4, pp. 374–382.
20. Gillies, D, et al. 2016, ‘Psychological therapies for children and adolescents exposed to trauma’, Cochrane Database Systematic Reviews, vol. 10, pp. Cd012371.
21. Kieling, C, et al. 2011, ‘Child and adolescent mental health worldwide: evidence for action’, The Lancet, vol. 378, no. 9801, pp. 1515-1525.
22. Fox, C & Hawton K 2004, Deliberate self-harm in adolescence, Jessica Kingsley Publishers, London 23. Guina, J, et al. 2017, ‘Should posttraumatic stress be a disorder or a specifier? Towards improved nosology within the DSM categorical classification system’, Current Psychiatry Reports, vol. 19, no. 10, pp. 66
23. Guina, J, et al. 2017, ‘Should posttraumatic stress be a disorder or a specifier? Towards
improved nosology within the DSM categorical classification system’, Current Psychiatry Reports, vol. 19, no. 10, pp. 66
24. Paus, T, Keshavan, M & Giedd, JN 2008, ‘Why do many psychiatric disorders emerge during adolescence?’, Nature Reviews Neuroscience, vol. 9, no. 12, pp. 947-57
25. Sayed, S, Iacoviello, BM & Charney, DS 2015, ‘Risk factors for the development of psychopathology following trauma’, Current Psychiatry Reports, vol. 17, no. 8, pp. 612
26. Brewin, CR, Andrews, B & Valentine, JD 2000, ‘Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults’, Journal of Consulting and Clinical Psychology, vol. 68, no. 5, pp. 748-66
27. Linley, PA & Joseph S 2004, ‘Positive change following trauma and adversity: a review’, Journal of Traumatic Stress, vol. 17, no. 1, pp. 11-21
28. Clay, R, Knibbs, J & Joseph, S 2009, ‘Measurement of posttraumatic growth in young people: a review’, Clinical Child Psychology and Psychiatry, vol. 14, no. 3, pp. 411-22
29. Tedeschi, RG & Calhoun LG 2004, ‘Posttraumatic Growth: Conceptual Foundations and Empirical Evidence’, Psychological Inquiry, vol. 15, no. 1, pp. 1-18
30. Weiss, KJ & Gutman AR 2017, ‘Testifying About Trauma: A Call for Science and Civility’, Journal of the American Academy of Psychiatry and Law, vol. 45, no. 1, pp. 2-6
31. van der Kolk, BA & Courtois CA 2005, ‘Editorial comments: Complex developmental trauma’, Journal of Traumatic Stress, vol. 18, no. 5, pp. 385-388
32. Widom, CS, Du Mont, K & Czaja, SJ 2007, ‘A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up’, Archives of General Psychiatry, vol. 64, no. 1, pp. 49-56
33. Fernandes, V & Osorio FL 2015, ‘Are there associations between early emotional trauma and anxiety disorders? Evidence from a systematic literature review and meta-analysis’, European Psychiatry, vol. 30, no. 6, pp. 756-764
34. Resick, PA, et al. 2012, ‘A critical evaluation of the complex PTSD literature: implications for DSM-5’, Journal of Traumatic Stress, vol. 25, no. 3, pp. 241-251
35. Ball, JS & Links PS 2009, ‘Borderline personality disorder and childhood trauma: evidence for a causal relationship’, Current Psychiatry Reports, vol. 11, no. 1, pp 63-68
36. Stevens, SJ, Murphy, BS & McKnight, K 2003, ‘Traumatic stress and gender differences in relationship to substance abuse, mental health, physical health, and HIV risk behavior in a sample of adolescents enrolled in drug treatment’, Child Maltreatment, vol. 8, no. 1, pp. 46-57
37. Pignatelli, AM, et al. 2017, ‘Childhood neglect in eating disorders: A systematic review and metaanalysis’, Journal of Trauma and Dissociation, vol. 18, no.1, pp. 100-115
38. Bendall, S et al. 2008, ‘ Childhood trauma and psychotic disorders: a systematic, critical review of the evidence’, Schizophrenia Bulletin, vol. 34, pp. 568-579
39. Miller, AB, et al. 2013, ‘The Relation Between Child Maltreatment and Adolescent Suicidal Behavior: A Systematic Review and Critical Examination of the Literature’, Clinical Child and Family Psychology Review, vol. 16, no. 2, pp. 146-172
Disclaimer
This information is not medical advice. It is generic and does not take into account your personal circumstances, physical wellbeing, mental status or mental requirements. Do not use this information to treat or diagnose your own or another person’s medical condition and never ignore medical advice or delay seeking it because of something in this information. Any medical questions should be referred to a qualified healthcare professional. If in doubt, please always seek medical advice.
Mythbuster writers
Anna Farrelly-Rosch
Dr Faye Scanlan
Youth contributors
Sarah Langley – Youth Research Council
Somayra Mamsa – Youth Research Council
Roxxanne MacDonald – Youth Advisory Council
Clinical consultant
Dr Sarah Bendall
First published as ‘Trauma and mental health in young people: Let’s get the facts straight’ by Orygen, 2018.

Resources
Excessive Exercise
Participation in regular physical activity is beneficial to both body and mind. It supports our body to grow stronger and our brain to work better. It relieves stress and anxiety and helps improve mood, concentration and memory.
However, when exercise becomes an obligation and you are experiencing negative consequences which put strain on your mind and body, there is a chance that you are exercising excessively, which can be a problem in itself, as over-exercising can bring serious negative impacts on health.
Why does it matter?
Excessive exercise affects both our physical and mental health. It could lead to potential injuries, due to overusing muscles or worsening previous injuries as your body is unable to recover fully. This could affect exercise performance in the longer term, especially among youth during this stage of physical development. Excessive exercise can also affect girls’ menstruation, as it directly and indirectly impacts hormonal changes in our bodies.
It can influence how you perceive your body, your self-esteem and it can be mentally taxing when our minds are preoccupied with the thoughts related to exercise. Excessive exercising can contribute to guilty feelings, or feelings of irritation and being on edge when you are not exercising. It also affects our daily lives and social relationship as we prioritise exercise over other matters.
Although it is not classified as a diagnosable mental health condition, over-exercising is often associated with multiple mental health conditions. Studies show that there is a link between excessive exercise, body dysmorphic disorder and eating disorders. It may also lead to or exacerbate existing mental health conditions, such as depression, anxiety, obsessive-compulsive disorder (OCD) and addiction.
Signs of excessive exercise
You may notice some of the following signs:
- Feeling prolonged muscle soreness and stiffness
- Feeling fatigued and tired, preventing you to maintain daily activities
- Feeling guilty for not exercising
- Constantly feeling the urge to exercise
- Finding your mind preoccupied with exercise and body image
- Using exercise as a key way to distract yourself from stress and anxiety
- Lower performance
- Unrealistically comparing yourself with others
- Often prioritising exercise over necessary tasks, social interactions and other urgent matters
Exercise is excessive and becomes a problem when it starts to affect your daily life and social relationships, or when it no longer brings you the benefits as originally intended. Reaching out to people you trust or seeking professional help can be useful.
What is the recommended amount of physical activity?
According to the World Health Organisation:
- Youth (aged 5-17) are recommended to do at least an hour of moderate to vigorous level of exercise per day. Adults are advised to undertake 150–300 minutes of moderate-intensity or 75–150 minutes of vigorous-intensity physical activity per week.
- Moderate level of physical activity – you can still talk, but you can’t sing, such as brisk walking and dancing
- Vigorous level of physical activity – you can only say a few words without stopping to catch a breath, such as running, hiking uphills, and jumping ropes
How can I take care of myself?
- Schedule rest days. Rest days are essential for your body to recover from exercising and strained muscles. It also lets you clear your mind from exercise and focus on other duties and work.
- Stick to an exercise schedule. Plan an exercise schedule that includes both active days and rest days.
- Take a break from exercise if you don’t feel like exercising. It is okay to take a break and let yourself recover from the accumulated stress from exercise – it can benefit you in the long run for your body and mind as they have time to recover to their optimal state.
- A healthy lifestyle is also crucial for your well-being as a whole. A healthy diet, sufficient rest and sleep also contribute to your physical and mental health. Learn more about maintaining a healthy lifestyle for your physical and mental well-being here.
- Talk to people you trust about your concerns. If you have concerns or struggle with over-exercising, talk to your friends, coach, teammates, or a family member you trust to see if alternatives are available. Talking to others is also a way to organise your thoughts and feelings.
- Engage in other activities. Engaging in other enjoyable activities can help focus on something else. If you find your mind is constantly occupied with exercise and related matters, try to immerse yourself in other enjoyable activities and enjoy the feeling that the new activity brings,
How friends and family can support
- Let them know you are worried and are there for them. If your loved ones show signs of excessive exercise that worry you, let them know that you care and are there to support and listen to them. Let them know that they are not alone.
- Acknowledge and validate their feelings and emotions. Different people hold different perspectives on things, and it is important to remember that all feelings and emotions are valid to their experiences. Avoid dismissing their worries and concerns, and try to understand their perspective.
- Don’t make assumptions. Excessive exercise can result from a mix of factors, don’t make assumptions about what drives them to exercise. Listening to them and understanding their perspective can encourage them to share more comfortably.
- Help them find useful information. Useful information such as maintaining overall wellbeing can encourage them to carry out healthy behaviours and avoid information that promotes unhealthy habits. It is also a way to show them that you care and are there to support them.
- Engage them in other activities. Spend time and engage in other enjoyable activities together, such as watching movies, online streaming, chatting and playing games.
Maintaining a healthy exercise habit can positively impact your life, both physically, mentally and socially – it is supposed to bring joy and relieve stress while keeping you physically healthy.
Reference
Trott, M., Yang, L., Jackson, S. E., Firth, J., Gillvray, C., Stubbs, B., & Smith, L. (2020). Prevalence and correlates of exercise addiction in the presence vs. absence of indicated eating disorders. Frontiers in Sports and Active Living. https://www.frontiersin.org/articles/10.3389/fspor.2020.00084/full
World Health Organisation. (2020). WHO Guidelines on Physical Activities and Sedentary Behaviour. https://apps.who.int/iris/bitstream/handle/10665/337001/9789240014886-eng.pdf.

Resources
Managing Disappointments Due to COVID-19
The COVID-19 pandemic has come with many challenges, one of which has been experiencing grief due to loss. The pandemic measures may have resulted in disruptions to our daily routines; separation from our friends and family; the missing of milestone events (like graduations, birthdays, vacations). We may also find that we feel guilty because we are grieving losses that seem less important than the loss of life. But our feelings of grief over the disruptions of the pandemic are valid, our losses may not be as important as the loss of life but they matter to us.
How do I know if the losses are negatively affecting you:
- Often feeling irritable, frustrated, angry or resentful
- Low mood
- Feeling generally unmotivated
- Being preoccupied with thoughts about what you are missing out on
How to manage feelings of grief
Acknowledge your feelings of loss and grief and find ways to express your feelings of loss and disappointment
- Journaling
- Expressing yourself through art: drawing, painting, music or dance
- Talking to friends or family about how you feel, sharing your feelings of disappointment and your concerns
Incorporate new rituales to your routine to replace ones that have been cancelled or have been put on hold.
- Exercise
- An interesting online course
- An artistic hobby – creative writing, drawing/painting/sculpting
- Cooking or baking
- Volunteering – there are lots of great volunteering opportunities that can be done remotely
Find creative ways to celebrate milestone moments (like graduations, birthdays, anniversaries)
- Creating creative videos with your friends/family to celebrate the moment
- Sending gifts or care packages and opening them together online
- Virtual celebrations
What creative celebration method can you come up with? Think outside the box!
Stay present. During this time of loss we may find ourselves worrying about future losses which can increase our anxiety and our frustration. Here are some ways you can stay present
- Mindfulness can help us ground ourselves in the moment allowing us to appreciate and savour the enjoyment we are experiencing. When practising mindfulness try using all of your senses to anchor yourself in the present moment.
Look around and notice- 5 things you can see
- 4 things you can physically feel
- 3 things you can hear
- 2 things you can smell
- 1 thing you can taste
- Savouring, this means to live in the moment and appreciate the moment. Great ways to savour are by capturing moments we are enjoying (photographing/drawing/painting), or journaling what we are grateful for

Resources
Supporting Young People Through the 5th Wave
Supporting Young People Through the 5th Wave
The current COVID-19 pandemic has been immensely disruptive to our young people; disruption to the school year and daily routines, separation from friends or family, postponement or cancellations of milestone events. Additionally, other stressors associated with the pandemic have been seen to negatively impact mental health wellbeing, such as uncertainty, alarming news feeds, and contradictory information. It is therefore important to help young people navigate these challenging times and foster resilience.
How to speak with your youth about the current situation
Start a conversation. Don’t shy away from talking about the challenges brought on by COVID19. Young people appreciate honest, open, non-judgemental conversations. What is unhelpful is to ignore or dismiss their concerns, this may drive them away from coming to you, and may lead them to seek answers and support on social media, which may not be as helpful and in some cases may be harmful.
Give them the space to explore how they are feeling and in turn how these feelings may be impacting the way they perceive the current situation as well as their behaviours, all in a non-judgemental environment.
Conversation starters:
“We are going through such difficult times, have you noticed any impacts on how you are feeling?”
“I have noticed that you have been down lately, is there anything you would like to talk about?”
“What is the hardest thing for you these days?”
Validate. Validate their feelings, showing them that you understand how difficult this has all been for them. Letting them know that “it’s ok to feel [sad/frustrated/angry] right now” can also help open a conversation about healthy ways to cope with these feelings. What is essential is to first listen to their concerns without jumping to solutions. Allow them to explore their feelings and letting them be heard first, before any exploration of solutions.
Provide reassurance. Discuss their specific concerns and provide reasurancess when possible. Exploring with them (it is important that this is something you do with them rather than telling them what to do) any strategies they can engage in to keep them safe and healthy. I.e. if they are concerned about getting infected, you can speak to them about helpful health supporting behaviours like washing hands, wearing a mask. This allows them to see that while some things are out of their control there are many things that are within their control.
Self-compassion. Reminding them to be gentle and kind to themselves. When we struggle we may have feelings of self-blame and self-criticism. Reminding them that these are challenging times and you are doing the best you can.
New routines. Encourage them and work with them to set a regular routine, replacing any cancelled/postponed activities with new engaging activities, and including health supporting behaviours such as:
- Regular bedtimes
- Exercise
- Connecting with friends and loved ones
- Engaging in a hobby or activity they are passionate about
Managing anxiety during COVID
The current pandemic has provoked anxiety in many people. While some anxiety can motivate us to protect ourselves and help keep us safe, if anxiety is not managed well it can impact day to day functioning.
Signs that a young person is struggling with anxiety:
- Preoccupation with their fears/worries
- Maladaptive coping behaviours (i.e. avoidance, substance reliance)
- Physical symptoms associated with their anxiety (which have been assessed by a GP but do not have physical origin) – i.e. headaches, muscle tension, pain, stomach discomfort
Supporting young people experiencing anxiety
Supporting young people who are experiencing anxiety will be through helping them to explore and recognise their anxious thoughts, validating their feelings and supporting them to engage in coping strategies. Supporting them to explore more measured ways to look at the situation. However, if they are having difficulties with this and their anxieties, seeking professional help will be helpful (more details on seeking professional support can be found at the end of this article)
Strategies:
- Help them to think of evidence to support their anxious thoughts and evidence that challenge their anxious thoughts. This will allow them to find a balance in their thinking and will help them challenge their anxieties
- Explore with them more optimistic ways of thinking about their situation – what is the upside
- Encourage them to practice mindfulness or grounding techniques which help bring us back to the present moment
Coping with isolation & low mood
The isolating nature of social distancing and school disruptions can lead to low mood and possibly depression, if helpful coping strategies are not used. Social contact and friendship development is an important developmental milestone in the adolescent years. Social connection disruption impacts both mood and healthy social development.
Signs that a young person is struggling:
- Low mood
- Further isolation, avoiding contact with friends
- Maladaptive coping behaviours (i.e. avoidance, substance use, self harm)
- Physical symptoms associated with their low mood (which have been assessed by a GP but do not have physical origin) – i.e. generalised pain, stomach discomfort
Supporting young people experiencing low mood
- Encourage them and support them to connect with friends and loved ones
- Allowing for more time on-line (within reason) on social platforms or gaming platforms that allow them to connect with their friends
- This is also a good time to speak to them about staying safe on-line
- Allowing for safe in-person meeting (within the limitations of social distancing guidelines)
- Help them set manageable expectations. Understanding that “good enough” and accomplished is better than perfect but not achievable, particularly during times of challenge
- Support them to explore hobbies or activities they can take up, to help them feel fulfilled and give them a sense of mastery and accomplishment
Seeking professional help
It is important to recognise when professional help is needed; such as speaking to a counsellor or psychologist to process experiences or engage in structured talk therapy. Many therapists are offering services virtually or have safety guidelines to help facilitate in-person therapy. To learn more about seeking mental health supports in Hong Kong follow the link here
How do I know a young person needs professional help?
- They are increasingly withdrawn, isolated or disengaged, and not responsive to coping strategies
- Engaging in self harm, substance reliance, or expressing suicidal thoughts
- Significant disruptions to their daily activities and engagement with the world around them due to their anxiety or mood
If you are concerned about safety or think your young person needs emergency supports please see the list of emergency services here
Taking care of yourself is essential during this time. You will not be able to effectively support others if you are struggling. The strategies above apply to your self-care as well, so ensure you are engaging in healthy coping strategies, this will also model healthy behaviours to the young person you are supporting.

Resources
What is Meditation?
What is mindfulness meditation?
- Mindfulness meditation is simply dropping down into our body & feeling the sensations of our body & our changing emotions.
- We are simply being present with what is going on inside us.
- We are anchoring ourselves in our present. Our thoughts no longer drive us to the past or the future, instead, we are fully living here.
Why is meditation important?
- Allows us to understand our mind and take control of it instead of having it control us. It brings inner peace and self awareness.
- Allows us to be present: to be aware of what is happening here and now: in our thoughts, our emotions, our bodies.
- Allows us to stop identifying with our thoughts and emotions.
- We have space to CHOOSE how to react, to CHOOSE the story we tell about ourselves.
How often should I practise?
- Start with a short meditation every day, five minutes of sitting down in the morning.
- Once you have a consistent habit, you may start to slowly increase the time you meditate for.
- Constancy over quantity
Benefits of mindfulness meditation
- Meditation helps you break out of negative thought patterns by giving you clarity.
- It can bring the simple peace and joy of being present, as you are less likely to repeat negative reactive patterns.
- The same way we have body hygiene, we need to have mental hygiene, to keep not just our body clean but our mind too.
- It is not just a personal responsibility but a collective one. When you centred and balanced within your mind, you spread that peace with everyone you meet through your own behaviour.

Resources
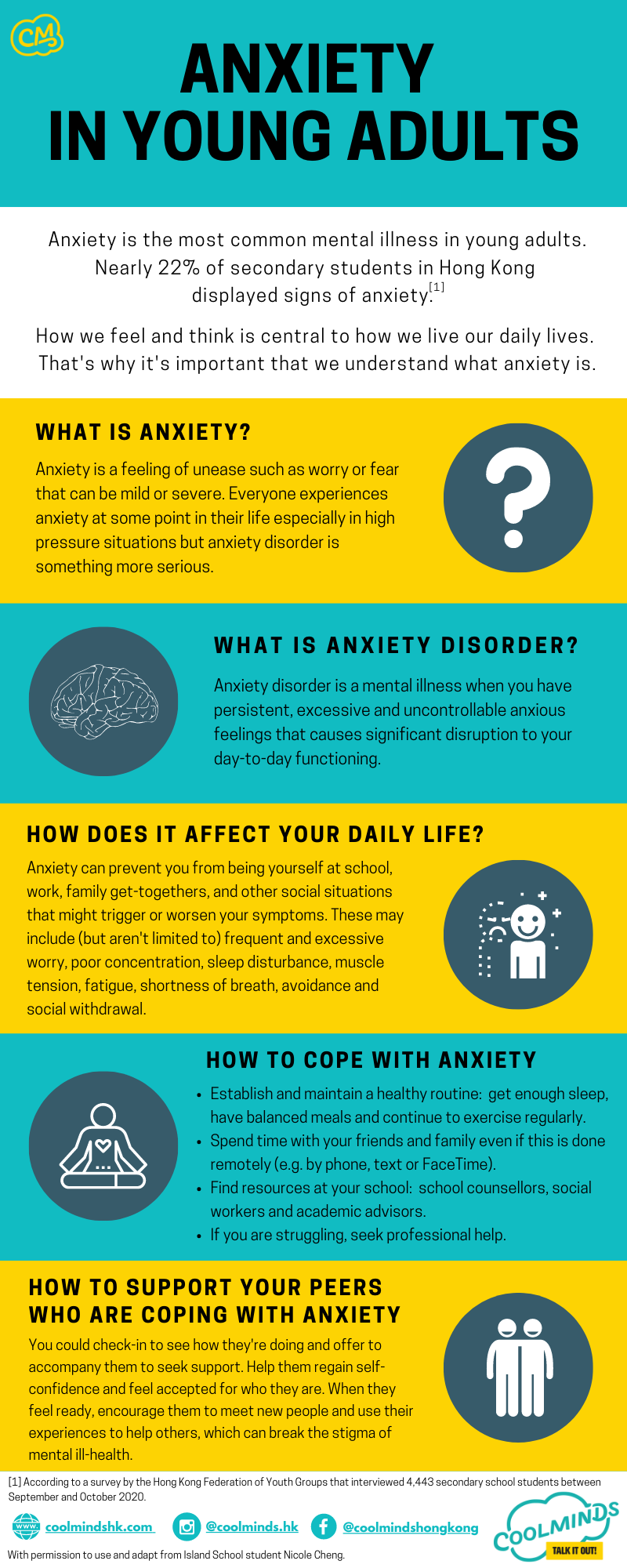
Anxiety in Young Adults
Anxiety is the most common mental illness in young adults.
According to a survey by the Hong Kong Federation of Youth Groups that interviewed 4,443 secondary school students between September and October 2020, nearly 22% of secondary students in Hong Kong displayed signs of anxiety.
How we feel and think is central to how we live our daily lives. That’s why it’s important that we understand what anxiety is.
What is anxiety?
Anxiety is a feeling of unease such as worry or fear that can be mild or severe. Everyone experiences anxiety at some point in their life especially in high pressure situations but anxiety disorder is something more serious.
What is anxiety disorder?
Anxiety disorder is a mental illness when you have persistent, excessive and uncontrollable anxious feelings that causes significant disruption to your day-to-day functioning.
How does it affect your daily life?
Anxiety can prevent you from being yourself at school, work, family get-togethers, and other social situations that might trigger or worsen your symptoms. These may include (but aren’t limited to) frequent and excessive worry, poor concentration, sleep disturbance, muscle tension, fatigue, shortness of breath, avoidance and social withdrawal.
How to cope with anxiety?
- Establish and maintain a healthy routine: get enough sleep, have balanced meals and continue to exercise regularly.
- Spend time with your friends and family even if this is done remotely (e.g. by phone, text or FaceTime).
- Find resources at your school: school counsellors, social workers and academic advisors.
- If you are struggling, seek professional help.
How to support your peers who are coping with anxiety?
You could check-in to see how they’re doing and offer to accompany them to seek support. Help them regain self-confidence and feel accepted for who they are. When they feel ready, encourage them to meet new people and use their experiences to help others, which can break the stigma of mental ill-health.
Special thanks to Island School student Nicole Cheng who granted permission to use and adapt her work.

Resources
Parents’ Guide to Navigating COVID-19
Efforts to stem the spread of COVID-19 through public health measures such as social distancing and self-isolation have taken a toll on Hong Kong’s youth. With prolonged school closures, many youth have increased their screen time and reduced their physical activity as well as face-to-face social interaction, which can contribute to low mood and loneliness. Changes in routine combined with the anxiety and stress associated with a new and unknown virus can lead to changes in behavior.
As a parent, it may be stressful to take care of both your own and your children’s mental health and wellbeing. This booklet aims to discuss how you, as a parent, can support your kids as well as yourself during these difficult times.
Talk it out
Talking to your young person about what is going on and why can help relieve some tension from both your and their minds. If you have noticed changes in your teenager, gently let them know what you have noticed and let them know there is no judgement. This is especially important to build trust. As parents, you are probably busier than ever, trying to manage work, home learning and other responsibilities. Therefore, it’s important to make a conscious effort to keep the lines of communication open.
Timing
Find a good time to talk, when you feel in a good headspace to do so and will be unlikely to be interrupted. If it’s not the right time, let your child know that you want to give them your full attention, and let them know when that will be.
Honesty
Be honest about what is happening in the world, and share only the facts to avoid unnecessary worries. It’s OK to say you don’t know the answer to a question and follow-up with the information later on or explain that there are many unknowns right now. Helping your teenager learn to sit with uncertainty is an important life lesson.
Active listening
Ensure that you are really listening to what they say, and let the conversation progress at their pace. Be a good listener, communicate that you respect their point of view, and validate what they are experiencing and their feelings. Remember, you can validate their experience even if you don’t agree with it or feel the same way. Offering reassurance or advice too quickly can have the opposite effect. Instead, focus on the idea of ‘listening without fixing’.
Shared resources
Let them know that there is help available and encourage them to talk to a doctor, other health professional, friend or family member if they need it. Do share a list of services designed specifically for young people in Hong Kong, which you can find on the Coolminds website.
Missed opportunities + Handling grief
Young people will likely face a lot of disappointments during this time such as missed school, parties, graduation, visiting universities, sports, and competitions for which they have prepared. As some of these are important milestones, it’s crucial to acknowledge these losses and the impact they have.
Let them know that it’s OK to feel angry, sad and frustrated, this may actually help them accept the disappointment.
Reassure them they are not alone and that, during this confusing time, many have been impacted and are also grieving for the losses caused by the pandemic.
Missing out on these types of events can also cause anxiety and low mood, so it is important to be on the look-out for that.
Here are some tips to help your young person cope with these losses:
- Stay connected
Find ways for them to stay connected to their friends. You may consider relaxing screen time rules to allow for this.
- Engage in personal expression
Journaling, drawing, painting, playing music, and dancing among others.
- Practising self-care
Ensure they get enough sleep and exercise, consider introducing meditation and/or yoga.
- Challenge negative thoughts
Reframe negative thoughts that might be out of proportion with less extreme and more realistic ones.
- Enjoying the wins
Some aspects of the situations such as missing classes they don’t like or activities they do not enjoy may be welcomed at this time, allow them to appreciate and celebrate these small “wins”.
- Continue the conversation
Don’t just check-in once, do so periodically as feelings and thoughts may change.
You might also feel a sense of sadness and grief at missing important milestones in your children’s lives. It is important to take the time to recognize your own disappointment and practise self-validation by acknowledging that these feelings are fair and valid despite seemingly bigger issues in the world. Take the time to grieve for these losses.
Youth mental health
It is important to understand that the measures we have to use to protect us from COVID-19 can impact our mental health. The fear of getting infected, uncertainty about the future, and all of the changes we’ve made to our routines can cause feelings of anxiety, while social distancing measures can lead to feelings of isolation and low mood. This is true for all of us and even more pronounced for those who have struggled with their mental health before the outbreak. It is therefore important to pay attention to your child’s mental health and wellbeing.
Normalise anxiety
Explain to them that anxiety is a natural feeling to have when there is a threat present, as is the case right now.
Discuss their perspective on the dangers involved and ensure that they are not overestimating the gravity of the situation or underestimating their ability to take care of themselves and manage difficult things.
Focus on strengths
Remind them that they are resilient and able to navigate tough situations. Remind them of different ways in which they have done so in the past.
Limit news exposure
Encourage youth to limit the amount of time they spend reading and watching information on COVID-19.
Remind them to refer only to reputable sources for updates.
Encourage helpful distractions
Such as watching movies, playing games, exercising and talking to friends. These can be used at times of distress or boredom.
Keep communication channels open
Encourage teenagers to discuss any concerns with family and friends.
Make sure that you are managing your own anxiety!
It’s possible that your kids are feeding off of you. If you are feeling particularly stressed, find someone to talk to or engage in an activity that usually helps you relax or calm down.
Youth may be especially frustrated with social distancing measures if some of their friends’ families are not participating in it. Explain that your family is doing what experts recommend and suggest that they blame you when telling their friends that they can’t go out. Remain open to suggestions as to how they can be social while remaining safe. Consider relaxing screen time rules to allow kids to connect with their friends online given they can’t always do it in person. At the same time, ensure that digital connecting does not replace in-person interactions with family, sleep or studying.
Don’t forget to give them time and space! Youth still need their privacy and alone time, especially with the increased togetherness created by working from home and no school. Don’t take it personally if they prefer to spend more time in their room, and do not give them a hard time about it as long as they are completing their school work and other responsibilities.
Self-care
Remember, in order to take care of your young person well, you need to take care of yourself first. Working from home or the office and trying to manage youth at home as well as home learning is hard. You may not be as efficient as you normally are. You may also feel you are not being the best parent you can be.
Be kind to yourself and give yourself a break, everyone is learning to navigate this new way of life, and it takes time to adapt and get things right. Keep in mind that spending more time together is not the same as the quality, focused time you probably have when you and your young person are accomplishing daily tasks separately.
Some self-care ideas include:
- Make time to switch off from responsibilities and duties every day. Read a good book or watch TV.
- Allow only a certain amount of time each day to learn about COVID-19 updates from reputable sources.
- Engage with family and friends on the phone, Facetime, Zoom, Whatsapp, etc.
- Schedule a date night with your partner or quality time alone with a friend at least once a week.
- Practise mindfulness. There are many free apps available to support mindfulness if you are unsure of how to do it.
This is also a time of uncertainty with regards to jobs and financial stability, which can cause high levels of stress and anxiety. Seek support from family and friends where possible. There are also some government sources that can be helpful.
Physical health
Exercise can boost our immune system but it also boosts our mood, our concentration, our confidence, and improves our sleep. Encourage your young person to engage in some form of physical activity every day. It is equally important for parents to do the same. This can be an opportunity to spend fun, non-stressful time together.
Get outside! Go for a run, bike ride or long walk. Take advantage of the many free exercise videos available online and through apps. Play video dance games and use virtual sports simulators. Use what you have in the environment around you to engage in physical activity. Getting your endorphins flowing will be beneficial for everyone.
It is also important to maintain a consistent sleep schedule to ensure you and your child get enough rest. Try your best to eat a healthy diet and drink plenty of water.
Home Learning
Home Learning is challenging for youth, parents and teachers alike. There are equipment and internet requirements to successfully engage in home learning. If you do not have access to these resources, talk to your school about how they can help you and your teenager accomplish what you need.
It is important to remember that your teenager is probably a lot more capable than you realise and can manage much of what they need to do on their own. Make sure to give them that credit and the opportunity to show you that they can do it.
Helpful tips: Routines & Schedules
- Draft a daily schedule together – make sure to get your teenager’s input instead of directing them. Empower them to be responsible for their time, which should allow them to get their school work done in addition to being “social” and engaging in other activities that are important to them.
- Try to use non-controlling, non-directive language to ensure teenagers are accomplishing what they need to, while communicating that they are still in control of their time. A good example of that is asking, “what is your plan today?” Agree on an amount of checking-in that is acceptable to both you and your youth. One idea is to schedule a window of time each day to check-in and provide any assistance that may be needed.
Try not to get stuck in thoughts about how you think youth will react and notice how they are managing. If they are acting more maturely than they have in the past, give them the autonomy to manage on their own accordingly.
Remember that most youth around the world are in a similar position. Your kids will most likely not be further behind others because of home learning. In addition, teachers are experts at managing such situations. They will help your child catch up when school resumes if necessary. For those who have kids graduating from secondary school or University, keep in mind that this is a global pandemic. Universities and employers are fully aware of the challenges faced during this time and the resulting repercussions for everyone. Keep in mind that this is not forever, kids will go back to school!
Use the extra time well!
Although the situation is far from ideal, families rarely get to spend this much time together so do not forget to enjoy it! Make time to do fun things together that you normally don’t have the time to do such as cooking, baking, playing board games, teaching a new skill, etc.
Give your closets and cabinets a good clear out, and donate things you no longer need to charity. Take the time to learn a new skill yourself. Take online classes if you are interested in a career change or to support your current line of work.
Most of all remember to look after yourself and your kids. Your mental and physical well-being are more important during this time than getting all of the school work done or being an exemplary employee. If you are feeling financially unstable, make use of government resources. If you or your kids are not able to maintain good mental health during this time using the suggestions provided, it’s important to seek professional help.
Emergency support
If you are experiencing strong levels of distress or trauma which are interfering with your life, remember that you do not have to face it alone, and that help is available.
For emergency support, please contact the hotlines below:
Emergency hotline: 999
The Samaritans 24-hour hotline (Multilingual): (852) 2896 0000
Samaritan Befrienders Hong Kong 24-hour hotline (Cantonese only): (852) 2389 2222
Suicide Prevention Services 24-hour hotline (Cantonese only): (852) 2382 0000
OpenUp 24/7 online emotional support service (English/Chinese): www.openup.hk
More support services can be found here: https://www.coolmindshk.com/en/emergency-hotlines/
More non-urgent support services can be found here: https://www.coolmindshk.com/en/communitydirectory/

Resources
Voices of Youth: Stigma, discrimination and mental health
Interviews with Khadeeja Khan and Zuhaa Khan, Coolminds Youth Summit Ambassadors, and Zita Marie Puentespina, a Year 10 student
What are your thoughts on how ethnic minorities view mental health, and how is this topic discussed?
Zita: Sadly, many ethnic minorities come face to face with the idea that mental health may be a taboo subject in their upbringing. Moreover, umbrella terms such as “being difficult” or “dramatic” may come into play. This helps delay an individual’s understanding of “mental health” and how they can healthily overcome it.
Khadeeja: I think ethnic minorities lack awareness when it comes to mental health. For many, if you cannot see it then it is not there. It is easier to visit a doctor for a bruise you have on your arm than visit the doctor for bruised emotions. In the ethnic minority community, mental health is seldom talked about and that only worsens it further. Common issues like post-natal depression in women are hardly ever discussed because the majority do not even know what it is and many do not know how to deal with it. Although the youth are a lot more open to this, parents can be ignorant to talk or even learn about mental health.
Name-calling and shaming with words like ‘mad’ , ‘crazy ’ , ‘attention-seeker’ are common in the minority community. Whilst doing my Psychology degree, I was faced with the same issues as it was considered a subject with ‘no future’ and ‘a waste of time’. So, while the youth are learning about mental health and are opening themselves up, the older ones are still closed off and driving the generation gap further apart. This is mainly because in the countries where the ethnic minority immigrants come from, mental health is a taboo, making it difficult for them to comprehend.
Zuhaa: Unfortunately it’s not prioritised and thrown under the radar for the most part, in my opinion. Until it becomes a visible issue (e.g. drug abuse and dependency). Depression, trauma, anxiety are often viewed as “excuses” and “acts of laziness” so the ones struggling from these challenges are far from receiving help in their own community. Success and making a name out of yourself is constantly deemed significant. As painful and discouraging as this may be, your status and success are measured by your bank balance and the number of properties you own in the EM community. There isn’t much talk about what’s going on in your head and the significance of emotional discomfort.
Issues with racism and discrimination reflect back to one’s identity. In the case of an immigrant child, the “sense of belonging” and “need for assurance ” are parts of life that the “average” local is provided with but immigrant children struggle to find. The use of labels and a lack of acceptance, appreciation, and respect can harm mental health and cause long-term detrimental effects on individuals.
As for personal experience, fortunately mine have been subtle compared to what others may have experienced. That said, hearing about troubling tales in your community can hurt your own mental health too. It adds to the emotional stress of constantly thinking “what this place, what do people presume of me” simply based off appearance, ethnic features, clothing etc.
What are some barriers for ethnic minorities who want to seek help?
Khadeeja: The main barrier is independence – many people live with their parents until they get married, so wanting to seek help under the guardianship of their parents would be difficult especially when the parents are not willing to agree or accept their mental health. Additionally, there is the issue of acceptance. Seeking help and being vulnerable would mean that they accept they are going through something and would have to be vocal about it, yet they have been taught to do the opposite their whole lives. Confidence plays a barrier too. When parents, family and society have told them to stay quiet and avoid their feelings, finding the confidence to speak out is hard and will need a lot of perseverance and support. Finally, confidentiality and trust is a huge barrier. Many ethnic minorities in Hong Kong are usually somehow acquaintances, friends or related to each other in other ways. The insecurity of information being ‘leaked’ to their parents, relatives etc discourages the youth and minorities as a whole about speaking up.
Zita: A barrier I believe is quite evident is the “communication barrier” as this does have an instant strain in one’s ability to express themselves and be fully understood. Although an EM may try their best to express their need for help, the receiving person may not understand them, despite the effort the EM may be showing. Due to prevalent language, cultural and inter-generational barriers, I believe acts of compassion and love should be shown louder.
How can we best support mental health for everyone despite cultural differences?
Khadeeja: We can make the ethnic minority community a safe place for them to open up. We can provide a platform for them which would empower them and help them. When other people from different backgrounds come together and speak out, it helps to de-stigmatize mental health and they can feel accepted and validated. We need to realise that although we may have different cultures, backgrounds and religions, the one thing that we can all connect with is our emotions and feelings. Education is vital too, and this should start from schools, which would then be brought to homes. Before I started my Psychology degree, I had minimal information about mental health. My education means that I can help others to get educated too. If we target 100 people, for example, we might not reach out to all of them but even if 50 parents can be educated on mental health, it may be enough to increase support around mental health for at least some people in our community.
Zita: We must have a constructive foundation in which a collection of knowledge about mental health is addressed and shared, this may be in different forms of media. This may be a place where individuals can share their own ideas and tailor the given resources to their own cultural backgrounds, as mental health should not take away from one’s culture but should be understood positively in the context of their culture.
Zuhaa: It’ s crucial to place significance on an individual’s culture since cultural influence does play a role in shaping one’s life. But we need to just set our differences aside and provide a set of ears to those who come to seek help. The fact is that there’s little to no emphasis on mental health in the community, all that there is is the constant denial of mental health as a health issue. This makes it so hard to speak up.
How can youth support other youth who have been victims of racism or discrimination?
Zuhaa: Remind them that it’s not their fault. Often times the discriminatory words and phrases used are a reflection of the racist himself. It’s a problem that is bred in the racist’s mind instead of the victim. At the end of the day, the victim needs to accept that it’s impossible to change one’s ethical features, the culture and custom they were born in. Spending more time in understanding one’s own culture and dwelling on its importance to the advances of the world are far better alternatives than constantly being hard on oneself because of an unfortunate encounter with racism. If possible, also advise the victims to be patient and try their best to spread awareness on what’s wrong and what shouldn’t be said to people from a different race, etc.
Khadeeja: Youth can support other youth who have been victims of racism and discrimination by speaking up about their own experiences. It’s that simple! We need advocates, ambassadors and supporters who can speak up about their own mental health experiences and this will encourage others to do the same. We need societies, groups and events by youth for youth and mental health Coolminds Youth Summit is a prime example of that! The youth can also just contribute their time to mental health charities and organisations and attend the events. The presence of youth at such occasions is enough to encourage other youth to get involved.
Zita: We must acknowledge their experiences, create a safe place for self-expression, and use these experiences to inform the immediate people around them in order to spread awareness. We must create a platform of understanding where people can become informed and then empowered to make a difference.
The lives of people with mental health conditions are often embedded by stigma as well as discrimination.
Stigma is a reality for many people with a mental illness, and they report that how others judge them is one of their greatest barriers to a complete and satisfying life.
Where to Get More Support
A List of Community Resources
Government Departments:
Support Service Centres for Ethnic Minorities – a list by the Race Relations Unit of the Home Affairs Department.
Integrated Children and Youth Services Centres – provide social work intervention for children and youth 6-24.
Integrated Community Centres for Mental Wellness – provide community support, social rehabilitation services, clinical assessment and treatment for those aged 15 or above and their family members or carers.
Government-funded Non-Profit Making Organizations (NPOs):
Christian Action SHINE Centre: Self-help and Mutual-help Groups for ethnic minorities who encounter social and economic problems.
Hong Kong Christian Service CHEER Centre: Counselling, guidance and referral services are provided by registered social workers for all ethnic minorities in Hong Kong and all organisations serving ethnic minorities, to facilitate their swift settlement in Hong Kong.
Hong Kong Community Network LINK Centre: Registered social workers offer counselling or referral to appropriate government department or agencies. Specially trained ethnic minority staff offer translation services.
International Social Service: Counselling and Guidance services for ethnic minorities with HKID cards.
New Home Association HOME Centre: Individual and mutual support for all ethnic minorities in Hong Kong.
Yuen Long Town Hall Support Service Centre for Ethnic Minorities: Provides counselling and referral service to pertinent organizations, offers emotional support, and gives sessions on problem-solving and stress management skills for Hong Kong ethnic minority residents aged 9-27.
The Zubin Foundation – Ethnic Minority Well-being Centre (EMWC)
The EMWC serves those in the ethnic minority community who would like to talk to a counsellor about their mental well-being. All counsellors are able to speak English plus Hindi/ Urdu. Counselling service is only available for individuals aged 16 or above. If you have not reached 18 yet, you are required to get your parents’ consent in order to receive our counselling service.
- Address: 5/F, Unit F-J, Block 2, Kwai Tak Industrial Centre, 15-33 Kwai Tak Street, Kwai Chung, Hong Kong
- Contact number: 9682 3100 (for enquiries on EMWC and making appointments) / 2540 9588 (general enquiries on The Zubin Foundation)
- Email: info@zubinfoundation.org
Yang Memorial Methodist Social Service – Yau Tsim Mong Family Education and Support Centre
Mutual help groups, individual and family counselling are provided for all ethnic minorities in Hong Kong.
- Address: 5/F, 396 Shanghai Street, Yaumatei, Kowloon
- Contact number: 2781 2921/ 6821 9115/ 6821 9114
- Email: ytmfesc@yang.org.hk
Christian Action (Woo Sung Street Centre)
Self help and mutual help groups for ethnic minorities who encounter social and economic problems.
- Address: 4/F., Lee Kong Commercial Building, 115 Woo Sung Street, Jordan, Kowloon
- Contact number: 3422 3820
- Email: emisc@christian-action.org.hk
The Salvation Army Yau Ma Tei Integrated Service for Young People
Focuses on growth and counselling, to foster a sense of belonging to Hong Kong among the ethnic minority group and help them adapt to life in Hong Kong.
- Address: 1/F Block 4, Prosperous Garden, 3 Public Square Street, Kowloon
- Contact number: 2770 8933
- Email: ymtis@ssd.salvation.org.hk
Emergency support
If you are experiencing strong levels of distress or trauma which are interfering with your life, remember that you do not have to face it alone, and that help is available.
For emergency support, please contact the hotlines below:
Emergency hotline: 999
The Samaritans 24-hour hotline (Multilingual): (852) 2896 0000
Samaritan Befrienders Hong Kong 24-hour hotline (Cantonese only): (852) 2389 2222
Suicide Prevention Services 24-hour hotline (Cantonese only): (852) 2382 0000
OpenUp 24/7 online emotional support service (English/Chinese): www.openup.hk
More support services can be found here: https://www.coolmindshk.com/en/emergency-hotlines/
More non-urgent support services can be found here: https://www.coolmindshk.com/en/communitydirectory/

Resources
Discrimination and Mental Health – A Guide for Young People
Introduction
Hong Kong is a very multicultural city with a melting pot of cultures. In the last 10 years, the number of non-Chinese ethnic people living in the city has increased by over 70%.
Did you know that ethnic minorities constitute 8% of Hong Kong’s population?
There are over half a million ethnic minorities living in Hong Kong.
72.2% of ethnic minorities aged 14 and below and 51% of ethnic minorities aged 15-24 were born in Hong Kong.
It’s important to understand that not everyone shares the same views and upbringing. What we see in the news, movies, social media, or books may present a very narrow or one-sided view of specific cultures. Diversity can help us work more productively in teams and foster creativity as there are lots of positive things we can learn from each other.
Learning about other cultures helps us understand different perspectives within our communities. It helps us challenge harmful stereotypes and personal biases about different groups. We can grow in understanding and learn to respect other “ways of being” that are not necessarily our own.
Unfortunately, not everyone fully understands and supports cultural diversity. Discrimination, racism, and stigma are still huge issues we face. This can take a toll on our mental health and the wellbeing of those around us.
What is discrimination?
Discrimination
Discrimination is unfavourable treatment based on underlying prejudice. It is referred to as unfair treatment due to a person’s identity, which can include the following:
- Age
- Sex
- Race
- Gender
- Colour
- Creed
- Religion
- Ethnicity
- Physical disability
- Family background
- Ancestry
- Gender identity
- Political belief
- Place of origin
- Mental illness
- Mental disability
- Nationality
- Family status
- Social status
- Citizenship
- Linguistic background
- Sexual orientation
- Monetary status
- Education level
Stigma is the negative stereotype and discrimination is the behaviour that results from this negative stereotype.
How does discrimination effect MENTAL HEALTH?
Impact of negative public attitudes
- Public misconceptions and increase in fear
- Justification of stereotypes
- Denial of jobs, friendships, relationships
- Loss of self-esteem, confidence
- Feeling weak
- Increase in stress levels
- Social exclusion and isolation
- Unwilling to seek help or speak to friends/family about problems
- Remains one of the greatest barriers to a satisfactory life
The lives of people with mental health conditions are often embedded by stigma as well as discrimination.
Stigma is a reality for many people with a mental illness, and they report that how others judge them is one of their greatest barriers to a complete and satisfying life.
Is discrimination a problem in Hong Kong?
What are some challenges ethnic minorities face in HK?
- Language barriers
- Lack of career opportunities
- Cultural differences
- A recent survey conducted by local universities revealed that 6 in 10 Hongkongers believe there is a prejudice against these ethnic minorities.
- Between 2013-2018, the Equal Opportunities Commission received a total of 397 complaints lodged under the Race Discrimination Ordinance.
- A study by the World Values Survey Association has shown that many Hongkongers would not want to live next to people of a different race.
Racial stereotypes are widespread in Hong Kong. They may be used in to discriminate in a range of areas, like law enforcement, renting accommodation, school admissions and opportunities for employment.
Due to discrimination, many ethnic minority youth feel that they are negatively perceived by the wider community. This may lead to over racism or micro-aggressions.
A study from the Zubin Foundation has found that due to discrimination and negative perceptions of ethnic minorities, many youth have felt “invisible”. For example, ethnic minorities are under-represented in advertisements and pop culture in Hong Kong. When they are featured, it is often in sources like the news where they may be portrayed as “criminals”.
“When I open the school doors in the morning, I would see some unpleasant faces. I guess some parents don ’t feel comfortable having me teach their kids.”
Lebo Mhlongo, a South African kindergarten teacher in HK, faces racism on a daily basis
References:
- South China Morning Post, “Is Hong Kong racist? Prejudice against ethnic minorities, especially Africans, undermines city’s claim to be truly international”, 21/7/2018
- South China Morning Post, “Racial discrimination is still an issue in HK”, 13/12/2019
- Zubin Foundation, “The Status of Ethnic Minorities in Hong Kong”, 2015
Where to Get More Support
A List of Community Resources
Government Departments:
Support Service Centres for Ethnic Minorities – a list by the Race Relations Unit of the Home Affairs Department.
Integrated Children and Youth Services Centres – provide social work intervention for children and youth 6-24.
Integrated Community Centres for Mental Wellness – provide community support, social rehabilitation services, clinical assessment and treatment for those aged 15 or above and their family members or carers.
Government-funded Non-Profit Making Organizations (NPOs):
Christian Action SHINE Centre: Self-help and Mutual-help Groups for ethnic minorities who encounter social and economic problems.
Hong Kong Christian Service CHEER Centre: Counselling, guidance and referral services are provided by registered social workers for all ethnic minorities in Hong Kong and all organisations serving ethnic minorities, to facilitate their swift settlement in Hong Kong.
Hong Kong Community Network LINK Centre: Registered social workers offer counselling or referral to appropriate government department or agencies. Specially trained ethnic minority staff offer translation services.
International Social Service: Counselling and Guidance services for ethnic minorities with HKID cards.
New Home Association HOME Centre: Individual and mutual support for all ethnic minorities in Hong Kong.
Yuen Long Town Hall Support Service Centre for Ethnic Minorities: Provides counselling and referral service to pertinent organizations, offers emotional support, and gives sessions on problem-solving and stress management skills for Hong Kong ethnic minority residents aged 9-27.
The Zubin Foundation – Ethnic Minority Well-being Centre (EMWC)
The EMWC serves those in the ethnic minority community who would like to talk to a counsellor about their mental well-being. All counsellors are able to speak English plus Hindi/ Urdu. Counselling service is only available for individuals aged 16 or above. If you have not reached 18 yet, you are required to get your parents’ consent in order to receive our counselling service.
- Address: 5/F, Unit F-J, Block 2, Kwai Tak Industrial Centre, 15-33 Kwai Tak Street, Kwai Chung, Hong Kong
- Contact number: 9682 3100 (for enquiries on EMWC and making appointments) / 2540 9588 (general enquiries on The Zubin Foundation)
- Email: info@zubinfoundation.org
Yang Memorial Methodist Social Service – Yau Tsim Mong Family Education and Support Centre
Mutual help groups, individual and family counselling are provided for all ethnic minorities in Hong Kong.
- Address: 5/F, 396 Shanghai Street, Yaumatei, Kowloon
- Contact number: 2781 2921/ 6821 9115/ 6821 9114
- Email: ytmfesc@yang.org.hk
Christian Action (Woo Sung Street Centre)
Self help and mutual help groups for ethnic minorities who encounter social and economic problems.
- Address: 4/F., Lee Kong Commercial Building, 115 Woo Sung Street, Jordan, Kowloon
- Contact number: 3422 3820
- Email: emisc@christian-action.org.hk
The Salvation Army Yau Ma Tei Integrated Service for Young People
Focuses on growth and counselling, to foster a sense of belonging to Hong Kong among the ethnic minority group and help them adapt to life in Hong Kong.
- Address: 1/F Block 4, Prosperous Garden, 3 Public Square Street, Kowloon
- Contact number: 2770 8933
- Email: ymtis@ssd.salvation.org.hk
Emergency support
If you are experiencing strong levels of distress or trauma which are interfering with your life, remember that you do not have to face it alone, and that help is available.
For emergency support, please contact the hotlines below:
Emergency hotline: 999
The Samaritans 24-hour hotline (Multilingual): (852) 2896 0000
Samaritan Befrienders Hong Kong 24-hour hotline (Cantonese only): (852) 2389 2222
Suicide Prevention Services 24-hour hotline (Cantonese only): (852) 2382 0000
OpenUp 24/7 online emotional support service (English/Chinese): www.openup.hk
More support services can be found here: https://www.coolmindshk.com/en/emergency-hotlines/
More non-urgent support services can be found here: https://www.coolmindshk.com/en/communitydirectory/

Resources
Seeking Help and What to Expect
Who to seek help from
Congratulations! If you are reading this section, that means you’re ready for change. But we know that seeking help can be confusing and overwhelming so let’s start by understanding what different mental health professionals do and how they can help. Here’s a guide on the range of mental health professionals that you may find:
General practitioner (GP)
General practitioners, also known as family doctors, are medical doctors specializing in general medicine. They are also the doctors you see when you are feeling physically unwell. Your GP is often the first professional you would see when you are struggling with your mental health. They are trained to assess, diagnose and treat mild to moderate mental health conditions. GP’s can prescribe medications and provide preventative care and health education. They can also refer and direct you to the appropriate specific mental health professionals. Seeing your GP is the best first step to getting help.
Psychiatrists
Psychiatrists are licensed medical doctors who specialize in mental health. They are trained to assess, diagnose and treat mental health disorders, primarily through prescribing and monitoring medication treatment, they often do not provide “talk therapy”. Your visit with a psychiatrist may include a blood test, a physical assessment and a risk assessment. Psychologists can work at hospitals, private offices, or community health centres.
Mental health nurse
A psychiatric nurse is a registered nurse with specialised training in mental health. A psychiatric nurse assesses, supports and advocates for care. They typically assist and work with psychiatrists working in the public health care system. As part of their role they follow up with patients regarding medications, and needed supports.
Social workers
Social workers are dedicated to helping people navigate and solve issues in their lives which may be caused by relationship problems, adjustment issues, traumatic events, or disabilities, etc. Through case management, they redirect clients to resources that best support them. Social workers can be found in a variety of settings, such as schools, private offices, hospitals, community health centres, and non-profit organisations.
Counsellors
Counsellors are masters-level professionals. They aim to help people to understand the complex social welfare system and help to access resources which support a person’s wellbeing. They also receive basic counselling training and may be able to provide counselling to people in distress. Counsellors can be found at schools, hospitals, community health centres, and in private practice.
So what’s the difference between a counsellor and a psychologist?
Psychologists often have more formal education who are trained to diagnose and treat specific mental illnesses, whereas counsellors help people to process and cope with their mental health struggles.
Clinical psychologists
In general, psychologists have doctoral training qualifications; however, they are not medical doctors and do not prescribe medication. Clinical psychologists are specially trained to diagnose and treat mental illnesses through talk therapy, and they are the most common type of psychologist you would see for a mental health issue.
Educational psychologists
Educational psychologists are trained in teaching and education, focusing on learning-related issues. They work with students, parents, teachers, and support professionals to help students in the school setting. Psychologists can be found in places such as private offices, hospitals, and schools.
Where to seek help
When seeking help for mental health issues, it can be intimidating or bothersome if we don’t understand how the system works. We gathered all the resources and made it as simple as possible to help you understand the differences between public and private healthcare systems when seeking help for mental health issues.
Public system
- Public clinics/hospitals have clinicians who are primarily local, with many who have completed their education and training in HK.
- Public services also tend to employ more short term therapists.
- Procedure: Based on Hospital Authority, the below is the general routine to find the right mental health professional help:
- Register an appointment to visit a general practitioner (GP).
- GP will refer you to a specialist as needed; assessments will be used to determine the urgency of the client’s case.
- Cost: It is very affordable to get the help you need through the public sector as the government does subsidise heavily. However, it is compromised with long wait times. See the next section for waiting time.
Private system
- From a cultural perspective private care is more aligned with western practices and culture.
- Private clinics/hospitals are more likely to have clinicians who have completed their education and training abroad.
- Procedure: You may get a referral from your GP OR you could also find a therapist on your own and schedule a consultation. If you decide to find your own therapist you will need to do some research to find a qualified therapist.
- Cost: Private is significantly more expensive, a reason why the majority of the population cannot seek help as they believe it is unaffordable. A 1-hour session can range from $1500 – $3000.
What to expect
So what should I expect before I head for my first session?
Before you head to your first session, remember this initial visit to a professional is no different than a first appointment with a new general practitioner (or family doctor). It may be uncomfortable to talk about some of your concerns and experiences but it is an important first step to getting better.
What will we talk about during first session?
However, a small detail that could cause anxious feelings is the fact that your relationship with a therapist is important to help your recovery journey. It could be intimidating to spill all your deepest and “darkest” secrets to a stranger you barely know and the thought of bailing might even cross your mind. Just know that every therapist actually understands the nerves of your feelings and they’ll try their best to soothe you and make you feel comfortable. Regardless, whether you’re full of nerves or can’t wait to start blabbing away on that couch, your new therapist will be ready for you and perfectly able to meet you where you’re at. And if all you want to talk about during that first session is how nervous you are or how much you don’t want to be there, then that’s totally fine.
How does talking with a professional help my condition?
There are many types of “talk therapies” available depending on the mental health issues you are struggling with. One of the most commonly used one is Cognitive Behaviour Therapy (CBT), which focuses on challenging and changing unhelpful thought and behaviour patterns, while improving emotional regulation and developing helpful coping strategies.
So what will happen in the first session?
In your first session, you may be asked about:
- Your mood, thoughts and behaviours
- Your lifestyle (friendships, school, intimate relationships, family relationships)
- Any recent events in your life that might be affecting your wellbeing
- Any changes to your sleep, diet and daily activities
- Your medical history
- If you are seeing a GP or a psychiatrist they may take your blood pressure, listen to your heart, as well as doing blood tests to explore any physical issues that may contribute to your emotions and behaviours
What about with a specific mental health professional? What questions do they ask?
With a specific mental health professional you may be asked:
- How long have you been experiencing these problems or issues?
- What have you tried to do to cope with it?
- What do you think the trigger could be?
- How often are you suffering from it?
- What was your life like before this issue or problem was present?
Are there any other questions they would ask? What should I do if I don’t want to answer certain questions?
There are many other questions that a therapist will ask once you start talking about your presenting problem. They’ll start out pretty general and get more detailed as the sessions move forward.
You’ll be asked to think about what’s going on and how you’re experiencing it. Some of it will feel really personal. A therapist needs to try to understand the triggers and causes of your struggles in order to figure out how they can help. If you ever feel like you don’t want to answer a question quite yet, speak up and say so.
With certain types of therapies or cases it may involve some homework. Just be aware that often therapy is most effective when you also put in the work outside of the office as well.
Often, a therapist will ask you what your goal is for therapy. It’s helpful to figure that out upfront. But it’s also okay if you don’t have a specific goal in mind when you start. There won’t be any pressure to try and define it early on.
- Types of therapy
- Confidentiality
- Your conversations with your therapist are confidential. However, if they are concerned about your safety or the safety of others they will talk to you about disclosing to a trusted supporter (usually your parent/guardian if that is safe).
- Goals of therapy
- Give you the tools and strategies for navigating whatever is going on in your life — from stress or relationship issues to managing a mental health diagnosis
- Process of therapy journey
- Length of treatment
- Touch on it may get worse before it gets better
- Mention every case is different, just because you are diagnosed with a psychological disorder does not indicate you can be generalised and treated like any other client that has the same condition as you.
- Relapse
- We don’t expect recovery to happen overnight, and sometimes it’ll bounce back, making you think you haven’t made any progress. But this is certainly not the case. One thing we want you to take away from reading this booklet is to take the first step of speaking up and seeking help.
Emergency support
If you are experiencing strong levels of distress or trauma which are interfering with your life, remember that you do not have to face it alone, and that help is available.
For emergency support, please contact the hotlines below:
Emergency hotline: 999
The Samaritans 24-hour hotline (Multilingual): (852) 2896 0000
Samaritan Befrienders Hong Kong 24-hour hotline (Cantonese only): (852) 2389 2222
Suicide Prevention Services 24-hour hotline (Cantonese only): (852) 2382 0000
OpenUp 24/7 online emotional support service (English/Chinese): www.openup.hk
More support services can be found here: https://www.coolmindshk.com/en/emergency-hotlines/
More non-urgent support services can be found here: https://www.coolmindshk.com/en/communitydirectory/

Resources
The Mental Health Effects of COVID-19 – A Teachers and Educators Guide
Introduction
Recent efforts to contain the spread of COVID-19 through public health measures such as social distancing and self-isolation have led to closures of schools and universities in Hong Kong, which was then followed by the rest of the world.
This severe disruption of missing the entire term and cancellation of exams have impacted students, parents and educators. Hence, these are the times to work together and continue providing the best optimal support system for the students and themselves.
This sudden and unexpected change in routine along with a considerable degree of fear, worry and uncertainty can lead to poor mental health, not to mention an increased risk of use in drugs or alcohol.
As a result of school closures, teaching had no choice but to shift online at a rapid and unprecedented rate, resulting in numerous challenges (e.g. technical issues, inability to interact with students).
In addition, the lack of concrete information and uncertainty regarding the course of COVID-19 has led to an evident spike in stress and anxiety for students and teachers. Students and adults alike who are used to being in school for 5 days may experience isolation and loneliness from social distancing.
This booklet discusses how teachers can support students and their own well-being during a crisis. It also touches on the role of E-learning and the important role it plays in maintaining communication between students and teachers. In addition, full interviews conducted with teachers in Hong Kong are included to get a first-hand perspective on the teachers’ role and perspective in the current situation.
Taking care of your own Mental Health and Wellbeing
Self-care
Self-care for educators is highly important. Educators should actively look after their own mental health and well-being and thereby effectively support young people.
The current crisis situation and the rapid switch to online learning has been a challenging time for teachers. Educators are developing new teaching environments, working autonomously and also managing their own family circumstances.
Professional self-care
- Regular supervision or consulting with a more experienced colleague
- Make a schedule with sufficient breaks
- Develop a peer-support group
- Understand boundaries between students and staff
- Read relevant journals and be mindful of the news and social media
Physical self-care
- Have regular sleep routine and healthy diet
- Take scheduled lunch breaks
- Use your sick leave if unwell
- Get some exercise before/after work regularly
Psychological self-care
- Keep a reflective journal
- Regular supervision or consulting with a more experienced colleague
- Turn off your email or phone outside work hours
- Take time to contact friends and family
Emotional self-care
- Take time to contact friends and family for support
- Engage in mindfulness practices like mediation (see Lazy 8 activity below)
- Read or watch non-crisis related entertainment
- Cultivate gratitude – write 3 good things you did each day
Supporting students during school closure due to a crisis
Hope
Hope refers to the feelings or expectations that everything will work out. In the current climate, students may feel discouraged, hopelessness, anger or anxiety. These feelings may last as the community continues to face uncertainty.
Students and adults both may feel lost without their usual social activities which may have been taken for granted before. Missing out on the social aspects of school such as sports, friends, competitions or performances may be leading to further hopelessness.
To encourage/stimulate a sense of hope, educators can:
- Have students connect with someone in their family or community to ask a person they respect how they stayed hopeful in troubled times
- Reference other historical times of crisis, including how these ended and how communities rebounded
- Encourage students to get fresh air and to exercise when possible
- Share stories of hope to inspire students to discover positive takeaways they can gain from this current crisis
Connections
Forming connections and networking plays an important role in relationships and the development of support systems. School closures, social distancing and closure of public facilities can lead to isolation and loneliness. Education can play a key role in making students feel connected.
To foster a sense of connectedness, educators can:
- Ask and discuss with students about something fun they did at home
- Greet students by name and create a touch-free or virtual routine (similar to a handshake, a hug or a high five)
- Put students in small groups for projects or activities, to keep up the social interaction online while working during their own time
- Foster a sense of community by use of group activities and projects
- Discuss directly the importance of putting in extra effort in connecting with others as we’re more prone to loneliness
Safety
Schools provide a safety net and comfort zone for students due to their structure. However, due to current events and school closure, students’ sense of safety may have been compromised. The constant change and unexpected events can lead to an increase in stress and anxiety. Educators should be aware that some families may also be experiencing career instability or financial issues– all of which can also have an effect on a student’s sense of safety.
Steps educators can take to support a sense of safety in students:
- Reach out, encourage students to connect in a safe space to discuss and safety concerns
- Encourage student to talk to their friends (see peer-support tips below)
- Encourage students to speak to their family members
- Go for family walks or hikes together
- Avoid watching/reading too much news, and only watch/read from reliable sources
- Try to maintain a regular family routine as much as possible
Transitioning to E-Learning
Educators in Hong Kong and now worldwide have made the rapid and sudden switch to E-learning. Below are some steps you can take right now to assist with the process.
Remember: Take this opportunity to be supportive to students and allow flexibility!
Communicate as early as possible!
Start communicating with students as soon as schools close so teachers can stay in touch immediately. Let them know that even though you’re not meeting face to face, the student-teacher relationship still exists.
Understand and communicate with students, understand that E-learning is a new and challenging process for all.
Identify a platform for E-learning
Many schools have already leveraged a platform during potential closures. If not, free platforms such as Google classrooms and zoom for video conferencing are free and relatively easy to roll out.
Establish clear expectations
Operating in an online manner can raise many questions for students, parents and educators who are used to face to face interactions. Here are some simple guidelines:
- Teachers, admin and the school IT support should be available during normal working hours
- Student classes take place at their scheduled times with flexibility for differing timezones
Maintain regular contact
Educators stress that maintenance of communication during implementation of the E-learning process is the most important! This does not just include communication between students and teachers, but also among staff members to check in and see how they’re doing.
Interconnectivity between staff is vital to check in and share resources. Key factor is that everyone should remain in the loop and on the same page as much as possible.
Go with the flow
Anxiety and stress levels will be high during school closures. Expect there to be conflicts in timetables, lack of motivation from students, and downtime in responses.
Educators will play a key part during this essential time as community members. Practice empathy towards students and the current situation. Encourage students to become independent while providing them the essential support.
Essential tips from teachers
- Don’t ignore the elephant in the room. If possible, talk about COVID-19 and fear of uncertainty. This is an opportunity for you to remind your students to consider the sources of their news and to beware of the large amount of misinformation.
- Let your students know that you are there for them and that if they need help, they can reach out to you.
- Humanise yourself and also have casual conversations during online lessons. Tell them your experience about how you’re dealing with the situation or any concerns you may have. Discuss with them how it has been “working from home” from a teacher’s viewpoint.
- Share something personal with them such as which book you’ve started reading, you’re doing an online course or working out at home
- If possible, create a community discussion board for students to share what is happening in their lives stress, fear or anxiety due to uncertain time
- Communication must always remain consistent!
- In addition to supporting students, continue to challenge them and provide them with sufficient work to keep them engaged academically.
- Repeat some of the lessons you taught in class if possible. This will help activate their memory of that lesson and being part of the community. This is highly important for students missing the classroom and social settings
- Remain optimistic! With everyday changes and news, stress levels are bound to be high. Emphasize everyone is in this together.
- Encourage peer-relationship building! Encourage all students to share phone numbers or social media details and support each other.
Interviews with Teachers
Tutor from University of Hong Kong
What are some ways the COVID-19 outbreak has affected students and young people?
I think the timing of the outbreak has now added more uncertainty and trust issues to the already pervading anxiety and low morale in young people. Hong Kong runs on economics, and the loss of jobs, cancellation of recruitment seminars in universities and medical advice on limiting meetings/social gatherings has also had a negative effect on mental health.
How are you as an educator coping with the situation and the concept of e-learning?
E-learning is definitely an emergent idea that has a lot of potential. People have already been learning from various courses on platforms like edX, Coursera, TED, Datacamp etc. However, there are some limitations on online teaching when it comes to accommodating topics which are practical/laboratory oriented, e.g. I teach Petrology and the practicals involve examining the rocks by hand and under the microscope. Practical and hands on experience has its challenges with E-learning. It is a challenging time for educators and students.
What can students do if they feel stressed about:
- Falling behind?
Fears of falling behind coursework can be quickly remedied. If there are genuine reasons, the universities do show leniency and do offer extensions. I think the current policy is offering two choices: (a) switching a course to a non-graded one OR (b) dropping course altogether (there is no add/drop deadlines) and then picking it up in a later semester. In general students can discuss this with the course instructors/ course coordinators and let them know if they are having problems. They have been instructed to be more considerate.
- Comparing themselves to friends/peers and feeling unproductive?
Pandemic or no pandemic, comparison with peers is not a good habit to get into and leads to stigma. In my experience every individual is unique in their own speed of learning and comprehension. Trying to get a fish to climb a tree and judging them for it is an ineffective thing. One should learn things on their own speed and be confident about it.
- Feeling lonely?
The easiest step in overcoming loneliness is also the hardest step: Talk with friends, family and classmates and open up to them about your concerns. It is very likely they will share you concerns. Discuss options and workarounds with people and solutions are bound to surface.
- Feeling disconnected from being a student/their teacher?
Yes, this might be problem to those people who are more attuned to conventional classrooms. We are trying to address any questions arising during the live lectures (slideshow + recordings + videoconferencing) and email until such time the normal function of the university resumes.
Can students email teachers with any questions they might have? Is it appropriate for students to reach out to teachers saying they feel stressed/have been struggling with their mental health?
Students can freely reach out their teachers with any queries they have with the coursework, but no specific instructions have been given to lecturers/teachers on dispensing mental health advice to students. Letting course instructors know of your situation is definitely a good idea though. It is most likely they will direct students to university therapists/counsellors/ university health service to manage the situation.
What are some tips you would have as a teacher for the student’s online learning experience? How can they study effectively at home?
Online learning can be a little distracting at times especially if you have other browser pages open alongside. I think the best way to avoid getting distracted is go take notes while the lecture is happening online and quickly ask questions to clear doubts. Make sure you keep cellphones away during the lectures and this would help too. As far as self-study is concerned, create a fixed daily routine with adequate breaks in between. And most importantly, when you finish studying, do other interesting things, build hobbies. The partitioning of work and non-work hours is critical to cognition and learning.
What are some quick and easy ways they can improve their mental health at home?
Read books, exercise, paint, garden, take walks (with masks on), and most importantly talk to family or friends. The feeling of being cooped up can be driven away when you immerse yourself in creative and productive activities.
What are some words of advice you would like to say to other teachers or parents reading this booklet?
Mental health issues cannot be solved in isolation by those suffering from it. Do not disregard a child’s/student’s concerns on coursework. If they are failing to submit assignments on time, check in on them and offer to help where help is needed. A judgement-free environment is quintessential. In many cases, if students are falling behind in coursework, it is not because they are lazy, but the fact that they are going through problems they are finding difficult to solve. Usually, a small push in the right direction really helps them produce the best work they can.
Teachers from International Christian School
What are some ways the COVID-19 outbreak has affected students?
Students are bored, unmotivated, lonely, worried. Many can’t even leave their apartments. They can’t do “normal” activities and spend as much time with friends. They’re stuck at home with their parents in a sometimes unpleasant way – everyone is feeling stressed and might be taking it out on each other.
Students have been thrown very suddenly into the “deep end” , a very steep and very sudden learning curve to cope is expected of them. They could be facing pressure from multiple sides: parents and teachers, and even themselves. Time management and self-discipline challenges, and isolation etc. compound to the issue.
- Difficulties coping socially, emotionally and physically due to decreased social contact (some students are only allowed outside once a week, or every two weeks), lack of structure and routine leading to lack of motivation and feelings of inadequacy.
- Extra stress of being in small quarters with the whole family for long periods of time, parents’ stress from going through SARS, parents’ stress with job impact/economic concerns/losing jobs and income.
How are you as an educator coping with the situation and the concept of e-learning?
I rely on email for most of my communication. I have zoom sessions once a week with each of my classes. We talk about their classwork, their stress levels, and sometimes play online games together. I have been overwhelmed with the amount of work it has been to chase students’ work. Sometimes it takes longer to track who has/hasn’t handed in work, send emails to them, find their parent’s email address, email the parents, etc…..than it takes to actually plan or mark their work.
I am very overwhelmed as an educator. It takes forever to write out every detail and instruction for lesson plans. It also takes time to create videos, google forms, google docs, slideshows, and other media for them, since they can’t see me give the examples or the instructions. There is a lot of differentiation involved to create meaningful work for all the different students. So lesson planning takes longer, but there is also so much more grading. The only way to know if a student has done the work you assigned is to check. So I am always always always always grading/checking/looking/emailing/filling out charts of missing work/updating gradebook, etc… All the while giving more and more assignments. It’s a seven day a week job.
- It has been a challenge to find relevant resources since the last time a similar situation like this happened would have been SARS. But SARS time did not have the technology we have now. So I think we’re quite fortunate as educators to be able to continue school online.
- The online learning protocol makes it difficult for some teachers to find the balance between helping their own children be successful with their online learning while providing online learning as a job for students, all while also trying to balance work/home life.
How would you describe this time in your career as an educator?
It has been frustration and boring, but I’m learning how to help students in a different way.
Challenging, monotonous, tiring, boring. I’m having to be much more creative and innovative than I normally would have to be. I feel discouraged, like I’m not doing enough even though I am so worn out. It’s forcing and giving me an opportunity to reevaluate what is true learning, and how to prepare students to be life-long learners. There might be a gap between the systematic approaches of school vs. learning, and philosophically and pedagogically, it’s a good time to reflect and perhaps rethink. This, coupled with an increased amount of work, is sometimes a reprieve, and sometimes discouraging, because there is a huge disparity that is incredibly dissatisfying. Someone said that it feels like we’re doing a whole lot more work to perhaps get a whole lot less learning in return.
- I think it has pushed me to find ways to support students virtually, when the work has mostly relied on face-to-face contact and relationship building.
- It’s been challenging to balance parenting and educating.
What can students do if they feel stressed about:
- Falling behind?
- Keep up with daily tasks. Communicate with teachers, do 1 thing to start, make a list and start crossing things off it as you complete them, make a schedule
- Be self-disciplined, and learn to understand consequences of their choices. Pacing is important.
- Use a planner/make a list of work to be done, prioritize work, communicate with teachers the need for more time or help
- Reach out earlier – don’t wait! – to teachers, counsellor and/or classmates who can help with support and practical help with school work/explaining things etc.
- The outbreak affecting their future?
- Focus on the “now” – take thoughts captive and seek guidance from others. Refocus thoughts on what is known, true and helpful, talk to someone about their worries
- Focus on the now, rather than worrying about the unknown and what might be. Focus on the things they have control over and only worry about those things
- Comparing themselves to friends/peers or feeling unproductive?
Know that many students and even teachers are struggling with the lack of routine and productivity. Try to give more compassion to the self, as this is an adjustment to everyone (not just Hong Kong but worldwide).
- Feeling lonely?
Call a friend; don’t just text them. Talking isn’t the same as being in person, but it’s better than just reading what’ s been written. Sometimes when I’ve felt lonely it has helped me to think that others probably feel the same way. Write messages to others thanking them for something, asking them how they are, or telling a story. Sometimes the act of helping others not feel lonely takes the feeling away from oneself.
Is it appropriate for students to reach out to teachers to say they feel stressed or have been struggling with their mental health?
Students need to be assertive and let someone know. Hopefully, students have an adult at school that they trust, whether it is a particular teacher or a coach. Teachers do the job they do because they care about students. Even if we are not trained to deal with a situation, we know how to connect that student to someone who is. Even just verbalising to someone who is trusted & won’t judge you can be a big step toward seeing things in a more positive light.
What are some tips you would give as a teacher for students’ online learning experience? How can they study effectively at home?
Complete the daily tasks. Leave the phone alone; set it in a different room and only use it during designated breaks. Know why you’re learning and doing what you’re doing so you stay on task and “work” becomes more meaningful.
Having done online learning myself in the past, I found that it is very easy to get behind and then almost impossible to catch up. Stay up to date if not ahead as much as possible. If anything is keeping you from completing work, write your teacher as soon as possible so they are aware.
Use a timer and set small goals for yourself. Chunk out the work into manageable steps.
What are some quick & easy ways students can improve their mental health at home?
Set a timer to take a break every hour. Walk around the room, look out the window, take some deep breaths. Also set a limit to how late you will work each day and keep a regular sleep routine. Give yourself small rewards and do things that you enjoy.
- Get up and move!
- Take a 2-minute break each hour to do some lunges and squats and jumping jacks to get your heart pumping. That will send blood to your brain and cause you to breathe deeply. Both will improve your mental health!
- Limit looking at/listening to TV or online news to once a day, and spend no more than 10 minutes doing it.
- Create a routine/structure/schedule and stick to it! Do it with a group of friends if it helps you follow it
- Get outside as much as possible – even a balcony or rooftop will help!
- Call friends, family in other countries that you don’t get to talk to very often
What are some words of advice you would like to say to young people reading this booklet?
This too shall pass. It’s not normal, true, but it’s not forever. Hang in there! These are the cards that we are dealt with. How you choose to play the cards and respond is up to you.
What advice would you have for parents to help their children out at this time and with e-learning?
Continue to monitor and provide boundaries for your child. Connect with your child and have meaningful conversations. Help them create a routine and structure. If your child needs extra help with certain subjects/planning that they normally would get in school but aren’t getting now, then you have to do it. Sit down with them every day.
- Go outside and exercise every day – even HK doctors say to do that for your physical and mental health!
- Listen. Don’t be too quick to speak or solve problems, sometimes they just need to verbalise and that’s all they need.
More time at home may lead to more conflicts with family. What are some tips for students to improve communication and parent-child relationships at home?
Communicate with the school to insist that all work from all teachers is done in a consistent way. All school work should be posted in a similar way or place. A spreadsheet with all the work in one place is helpful. This may cut down on frustration, and parents feeling like they don’t know how to find what their kids need to do.
Joe M. – High school English Teacher
How are you as an educator coping with the situation and the concept of e-learning?
The current climate calls for colleagues and teachers to help each other. The non-traditional way of education is changing, it is not going to be perfect. Students will not be afraid of making mistakes if teachers are the same. I understand that learning is a lifelong process and it is okay to make mistakes or we’ll stagnate and this applies in all fields.
I found it is important to check with other teachers and see in what ways they are adapting. It’s also important to see how much work they’re giving so the students are not overburdened.
Would you describe this as a challenging time in your career as an educator?
Yes really interesting as it forces educators to look at the technological tools as we already have our way of doing things so we’re less open to electronic tools. I’ve been teaching for 25 years and this has been the biggest transition. The younger years are more welcoming to come on the camera than the older ones. Hence, working with growing adolescents combined with E-learning and technology has further implications.
I found the young people are very adaptable as per the situation. They’re very well versed with technology and problem solving.
What is your advice to students and teachers during the current period?
Students have different personalities and hence cannot be grouped together. As a teacher I need to understand that young people are stressed about a variety of factors such as academics, social interactions, conflicts, and the future.
Studying from home has allowed students to become autonomous. I’ve noted that the older students are liking the aspect of independence and organising and scheduling their own schedules. I have noticed that individual work has improved including their English writing and comprehension. Hence, as a teacher I firmly believe young people have the ability to show great resilience during tough times and change.
Speaking of giving young people autonomy, I’ve taken away the concept of deadlines but focused on giving them day to day work and focus on discussions. Some students have complained that they’re in fact getting extra work now as teachers are giving them more assignments for grading. Hence it is important to adapt and listen to what students are saying so we can all work together.
Students are really missing the social aspect of school. This serves as a great opportunity and rare change for parents to really bond with their children!

Resources
Asking for Help
When it’s time to talk about your mental health
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
We would like to acknowledge the Charlie Waller Memorial Trust (CWMT) UK for these resources and for allowing us to adapt this. For the original version of this resource, please refer to the CWMT website: www.cwmt.org.uk
Find out who’s best to talk to
You might already know who you want to talk to, perhaps a parent or a teacher you get on especially well with. If you’re not sure who to talk to then it’s worth thinking about who you trust and feel comfortable talking to. Have you talked to someone who has been particularly helpful before?
Think about what you want to say
Whilst you may have made the decision to talk to someone, you still need to decide what you want to tell them. You might want to think about:
- Is there a problem you need to talk about?
- How much are you happy to share?
- How do you feel each day?
- What has prompted you to ask for help now?
- Is there anything you are finding hard to manage?
Practise saying what you need to say
It’s alright to be nervous, so it’s a good idea to prepare. It sounds a bit strange but you’ll feel much more confident talking to a parent or teacher if you’ve worked out what you want to say and tried saying it beforehand.
You can start by writing down bullet points, writing a text or using a free online resource called Doc Ready… You could give this to someone to read if you are not yet comfortable to talk.
It’s worth writing a list of what you want to say to take with you so you don’t forget anything. You could formulate your words into a letter, both to help you work out what to say and also as a back- up. That way if you find yourself unable to talk about your issues you could give the letter to the person you’ve chosen to talk to instead.
It’s ok to start small and say ‘I’m not having a good day’.
A good next step is to call an anonymous helpline (see ‘Sources of advice’ for local helplines) and practise talking to someone you don’t know – that can be easier than talking to someone you know and care about and can help you whilst you get ready to take the next step.
Find a quiet time
Make sure you start the conversation at a time when the person you’re talking to won’t be interrupted and has time to listen to you properly. It’s important not to rush the conversation. If they can’t talk now, it doesn’t mean they don’t care about you; ask them when would be a good time to talk and come back then.
Take it slowly
Don’t feel like you have to say everything in one breath, or even in that first conversation. Take it nice and slowly and don’t be afraid to pause to think about what to say next.
Don’t over-analyse their reaction
It’s perfectly normal to try and second guess what the person you’re talking to is thinking. You might have all sorts of ideas about what is going through their mind, but don’t try to second guess. They might be surprised, and thinking of ways and routes to help. Try to ask them rather than just guessing.
Remember that there are other people to talk to if the conversation doesn’t go as well as you hoped.
It’s okay to cry
However you react, it’s ok. It’s natural to cry or feel angry. None of these feelings are a bad thing.
Know your rights about confidentiality
If you talk to someone who you know through their professional role, one of the first things they’ll do is to tell you that they can’t keep confidentiality. That’s because they’ll need to ensure you get the support you need to help you to get on top of things.
You can talk to them about who needs to know what – but try to remember it’s a good thing that people understand what’s going on so they can help you, though it might seem a bit scary at first.
Think about what you want to happen next
It’s a big step to ask for help and it usually means that on some level you’re ready for things to improve. Do you have any idea of what you might like to happen as a result of the conversation you’re planning? This might include:
- Support telling parents or a friend
- First aid or medical help for injuries
- Support to help you talk through and overcome underlying issues
- Referral for specific treatment that you’re already aware of (or learn more about possible available treatments)
- You’re not sure, you just can’t carry on with how things are
Even if you’ve gone looking for help, it can be hard to accept it – but try. Have faith in the person you’ve confided in to help you to take the first steps to make things better. They won’t be able to fix everything all in one go, but they can work with you to start to make things change.
“When I first started talking I realised I wasn’t so alone”
“From the moment I took that brave step I felt very much less alone.”
“I thought it was weak to ask for help, but I realised eventually that it was the ultimate sign of strength.”
“You’re not alone. Reach out… let yourself be loved.”
“Although it can be hard to take a first step there is help out there”
Sources of advice (Hong Kong)
Bilingual Telephone Hotlines
Samaritans Hong Kong 24-hour hotline: 2896 0000
Samaritan Befrienders Hong Kong 24-hour hotline: 2389 2222
Suicide Prevention Services 24-hour hotline: 2382 0000
Suicide Prevention Services “Youth Link” hotline (available 2pm-2am): 2382 0777
Hospital Authority Mental Health Direct hotline: 2466 7350
Chinese-Only Telephone Hotlines
Youth Outreach 24-hour hotline service: 9088 1023
The Hong Kong Federation of Youth Groups “Youthline” hotline (available Mon-Sat, 2pm-2am): 2777 8899

Resources
No Harm Done: Recognising and Responding to Self-Harm
Next steps for staff working with young people
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
We would like to acknowledge the Charlie Waller Memorial Trust (CWMT) UK for these resources and for allowing us to adapt this. For the original version of this resource, please refer to the CWMT website: www.cwmt.org.uk
INTRODUCTION
Self-harm describes any way in which a young person might harm themselves or put themselves at risk in order to cope with difficult thoughts, feelings or experiences. It affects up to 1 in 5 young people and spans the divides of gender, class, age and ethnicity. As such, many people find themselves in the position of wanting to support a young person who is self-harming. This can be difficult due to lack of confidence or uncertainty about what to say or do. Here we’ve provided simple guidance for taking those first steps – your support can be life-changing.
“I was so alone and lost and desperate. I thought no one cared until my [social worker] encouraged me to open up. I remember that day so vividly – it was the first day of the rest of my life.”
SELF-HARM WARNING SIGNS
There are many signs you can look out for which indicate a young person is in distress and may be harming themselves, or at risk of self-harm, the most obvious being physical injuries which:
- you observe on more than one occasion
- appear too neat or ordered to be accidental
- do not appear consistent with how the young person says they were sustained
Other warning signs include:
- secrecy or disappearing at times of high emotion
- long or baggy clothing covering arms or legs even in warm weather
- increasing isolation or unwillingness to engage
- avoiding changing in front of others (may avoid PE, shopping, sleepovers)
- absence or lateness
- general low mood or irritability
- negative self-talk – feeling worthless, hopeless or aimless
“At first we thought he was just accident prone, it was easy to miss, he always had an explanation as to how he’d got hurt.”
THE FIRST CONVERSATION
The sooner we encourage a young person to disclose their self-harm, the sooner we are able to provide or seek appropriate support to help them break the cycle. We can do so by passing our concerns on to a [trusted adult/teacher] or by providing a safe space for the young person to talk to us.
“It was the hardest conversation of my life, but every word I spoke made the load feel a little lighter and for the first time in a long time, I felt hope.”
The most supportive first conversation is one where:
- the young person is the sole focus of your attention
- you spend most of your time listening, not talking
- the young person tells their story, you never guess or assume
- there is a feeling of acceptance and support, not judgement
- self-harm is not dismissed as attention seeking
- unrealistic promises are not made about confidentiality
- this is recognised as the first step of a difficult journey
- clear next steps are identified and followed up promptly
- you recognise how hard this conversation must be for the young person
- you respond calmly – even if you don’t feel calm
“I’m not looking for attention, it’s just the only thing that helps me control the wayI feel.”
WHEN A YOUNG PERSON ISN’T READY TO TALK
When a young person is more reluctant to disclose or discuss their self-harm, three important questions to consider are:
- Who is the best person to have this conversation? You can use your knowledge of the young person, or ask them who they feel comfortable talking to.
- How can you help the conversation flow? An informal environment or talking whilst carrying out another activity such as walking or drawing can really help.
- Would another medium work better? Some young people feel happier talking via instant messenger, text or email – be creative and use your knowledge of the child.
“I tried several times to talk to him to no avail; it was only when I texted him that the conversation finally started.”
If a young person still isn’t ready to open up, provide them with details of anonymous sources of support and regularly revisit the situation.
“The [phone] counsellor helped me get more comfortable talking about things and next time my teacher tried to talk to me, I felt ready.”
NEXT STEPS
If you have any concerns about a young person’s immediate safety, this is an absolute priority and should be treated as an urgent safeguarding issue in line with your policies. If you think a young person is at risk, they should not be left alone.
All discussions should be recorded and shared with a trusted adult/teacher who will keep these details on file and can provide support and direction on appropriate next steps. These might include:
- Informing adults who need to know in order to keep the young person safe. This will usually include parents or carers.
- Visiting the GP to seek further support and guidance.
- Providing access to a school counsellor.
- Setting up regular meetings with a trusted adult such as a class teacher who can provide practical support and guidance.
It is important that all wounds are appropriately dressed and cared for as infection is common. Provide the young person with information about wound care or access to a trained first aider or medical professional who can assess and dress any wounds.
“He didn’t want to show me his wounds but he was happy to have the school nurse assess and dress them as long as I told her not to ask any questions.”
PROVIDING PRACTICAL SUPPORT
If you find yourself in the position of providing regular support to a young person, here are some helpful things you can do:
Listen – provide a safe space for non-judgmental, supportive listening. Even a few minutes of high quality listening can make a huge difference to how supported a young person feels.
Address stressors – work with the young person to understand their triggers and stressors. Working through a typical day and highlighting the tough bits can be a great way to start and then think creatively of ways you might address these.
Make a self-soothe box – work with the young person to collect a range of different things they can use to distract or soothe themselves when they feel the urge to self-harm. This might include music, colouring, books, bubbles, photographs or inspirational quotes.
Provide safe sources of further information – highlight sources of further information such as those listed at the end of this resource.
Safeguarding your own wellbeing – It can be emotionally challenging to support a young person who is self-harming so it’s important that you too receive regular support and confidential listening. Keep in regular contact with a trusted adult/teacher and if, for any reason, you feel you are unable to continue to support the young person, discuss this at the earliest opportunity.
“Things changed for me at home and I felt unable to provide the level of support she deserved. I was honest with her and we identified a different adult she could regularly speak to.”
WHOLE SCHOOL APPROACH
Whilst there is much that proactive, supportive individuals can do to help a young person within their school or organisation, this support is best provided within the context of a whole school approach in order to keep both ourselves, and the young person as safe as possible. Simple steps that your school could take include:
1. Developing and implementing a mental health policy
Clear guidance can give staff the knowledge and confidence they need to respond to issues appropriately. It is important to develop a policy that feels relevant and achievable within your setting and to ensure that all staff know who to refer to with concerns.
2. Providing training for all staff
Providing basic training for all staff on how to recognise and respond to self-harm will increase the confidence of both staff and students in making and responding to disclosures.
3. Addressing self-harm as part of the curriculum
Your school curriculum can provide a great opportunity to tackle myths and misunderstandings surrounding self-harm and to provide students with an understanding of how to keep themselves and each other supported and safe.
4. Looking after staff wellbeing
Before we can look after others, we must first look after ourselves. Supporting young people who are in emotional distress can be physically and mentally draining for staff; this needs to be recognised and appropriate support put in place, both in terms of training and supportive listening.
“Most importantly, the [professional training] day got us talking about self-harm. It was uncomfortable at first but we all grew in confidence throughout the day. It was really empowering – we’re no longer scared of disclosures, we feel confident we can help.”
FURTHER INFORMATION (UK-only)
YoungMinds: youngminds.org.uk Parents Helpline 0808 802 5544 (Monday to Friday 9.30am – 4pm)
YoungMinds provides information and free resources to help implement a whole school approach and self-harm, mental health and resilience training for professionals.
Charlie Waller Memorial Trust provides free self-harm training to staff working with young people.
Factsheet from The Royal College of Psychiatrists Childline: childline.org.uk 0800 1111 (24hr)
Helpline (24 hr): 08457 90 90 90 UK & NI
Email: jo@samaritans.org The Site: thesite.org
Self-Harm Alternatives: over 130 ideas for use in recovery suggested by young people, collated by Dr Pooky Knightsmith
Self-Harm and Eating Disorders in Schools: A Guide to Whole-School Strategies and Practical Support by Pooky Knightsmith. Available as a paperback or Kindle
A Short Introduction to Understanding and Supporting Children and Young People Who Self-Harm by Professor Carol Fitzpatrick. Available as a paperback or Kindle
No Harm Done: film & resource pack for parents
No Harm Done: film & resource pack for young people
“There’s no denying that it’s a gruelling journey and there are downs as well as ups; but once you’re out the other side and you see a happy, healthy young person ready to head out into the world it is the best feeling ever.”

Resources
Seeking Help for Anxiety
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to the Black Dog Institute for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to the Black Dog Institute’s website: www.blackdoginstitute.org.au
What this fact sheet covers:
- Why seek help for anxiety?
- Who to talk to
- Treatment available
It’s important to get treatment for anxiety
Anxiety is physically and emotionally exhausting. Getting help early means you can start to get relief and recover sooner. There are many professionals who treat all kinds of anxiety.
There is a wide range of effective treatments for anxiety, e.g.
- Cognitive behavioural therapy (CBT)
- E-mental health tools
- Relaxation techniques
- Medications
There are also lots of things you can do to help yourself.
Often, it’s a combination of things that help us get better, such as:
- A well-informed health professional you feel comfortable talking to
- The right psychological and medical therapies
- Support from family and friends
- Exercising and healthy eating
- Learning ways to manage challenges and stress, such as structured problem solving, meditation and yoga
How do I know it’s anxiety?
Severe anxiety can appear in ways that feel like other health issues, e.g.
- Chest pain
- A racing heartbeat
- Dizziness
- Rashes
Sometimes, anxious people think they’re having a heart attack.
When we’re anxious, we can also become hyper-aware of:
- Our body
- Aches and pains
- Perceived threats and danger
Sometimes, once we’re aware of a problem, we can become ‘hyper-vigilant’ in checking on all the discomforts and pains we feel. This can spiral into feeling more concern and worry, making the anxiety more severe.
You should always see a doctor, so they can make a thorough check of your symptoms and rule out any other medical condition.
Who can provide help for anxiety?
As well as your doctor, there are other health professionals who can help with anxiety, including:
- Psychologists
- Psychiatrists
- Counsellors
- School and university counsellors
- Social workers and occupational therapists trained in mental health
- Mental health nurses
What type of treatment is available?
There are three broad categories of treatment for anxiety:
- Psychological treatments (talking therapies)
- Physical treatments (medications)
- Self-help and alternative therapies
Psychological therapies are the most effective way to treat and prevent the recurrence of most types of anxiety. Depending on the type of anxiety, self-help and alternative therapies can also be helpful. They can be used alone or combined with physical and psychological treatments.
A thorough assessment by your doctor is needed to decide on the best combination of treatments for you.
Psychological treatments
Psychological treatments can be one-on-one, group-based or online interactions. Psychological treatments are sometimes called ‘talking therapies’ as opposed to ‘chemical therapies’ (i.e. medications).
Talking therapies can help us change habits in the way we think, and cope better with life’s challenges. They can help us address the reasons behind our anxiety, and also prevent anxiety from returning.
There are a wide range of psychological treatments for anxiety, including:
- Cognitive behaviour therapy (CBT)
- Exposure therapy (behaviour therapy)
- Interpersonal therapy (IPT)
- Mindfulness-based cognitive therapy
- Positive psychology
- Psychotherapies
- Counselling
- Narrative therapy
Some of the above treatments can be accessed online. Evidence-based online treatments can be as effective as face-to-face treatments. These online treatments are often referred to as e-mental health programs.
Physical treatments
Your doctor should undertake a thorough health check before deciding whether medication is a good option for you. Taking medication for anxiety must be supervised by a doctor. If medication is prescribed as part of your treatment, your doctor should explain the reason for choosing the medication they’ve prescribed.
Your doctor will:
- Discuss the risks and benefits, side effects, and how regularly you need check-ups.
- Advise what treatments can work together with the medication, such as psychotherapy, lifestyle changes (e.g. exercise) and other support options.
Anti-anxiety medications are used for very severe anxiety in anxiety types such as:
- Panic disorder
- Generalised anxiety disorder (GAD)
- Social phobia
Anti-anxiety medications, such as benzodiazepines, can:
- Be addictive
- Become ineffective over time
- Have other side effects such as headaches, dizziness and memory loss
Anti-anxiety medications are not recommended for long-term use.
It’s important to know that not all anxiety needs medication. Many people respond well to lifestyle changes and psychological treatments.
Self-help and alternative therapies
There are a wide range of self-help measures and therapies that can be useful for anxiety. It’s good to know that there are things you can do for yourself to feel better.
Self-help and complementary therapies that may be useful for anxiety include:
- Exercise
- Good nutrition
- Omega-3
- Meditation
- De-arousal strategies
- Relaxation and breathing techniques
- Yoga
- Alcohol and drug avoidance
- Acupuncture
Different types of anxiety respond to different kinds of treatments. Severe anxiety may not respond to self-help and alternative therapies alone. These can be valuable adjuncts to psychological and physical treatments.
e-mental health programs
e-mental health programs can be used in conjunction with a mental health professional or as a stand-alone option. e-mental health programs (also called ‘e-therapies’ or ‘online therapies’) are online mental health treatment and support services. You can access them on the internet using your smartphone, tablet or computer. The programs can help people experiencing mild-to- moderate depression or anxiety.
Some e-mental health tools, such as myCompass developed by the Black Dog Institute, have been found to be as effective in treating mild-to- moderate depression as face-to-face therapies.
e-mental health treatments are based on face-to-face therapy, positive psychology and behavioural activation. These therapies mainly focus on reframing thoughts and changing behaviour.
Key points to remember
- Lots of professionals can help you with anxiety
- There are many types of treatments for anxiety, and you can get better
- Many people who have had anxiety have been able to seek help and live active, fulfilling lives
Contact Us
Coolminds
Email: hello@coolmindshk.com
Black Dog Institute
Email: blackdog@blackdog.org.au
Where to get more Information and Support
Black Dog Institute – “myCompass”
Student Health Services – “Understanding Anxiety Disorders”
OCD & Anxiety Support Hong Kong
Mind Hong Kong – “Anxiety and Panic Attacks”
The Mental Health Association of Hong Kong:
Phone: 2528 0196
Website: www.mhahk.org.hk

Resources
Helping Someone Who Has a Mental Illness: For Family and Friends
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to the Black Dog Institute for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to the Black Dog Institute’s website: www.blackdoginstitute.org.au
What this fact sheet covers:
- How to tell if someone has a mental illness
- What to do if you are concerned about a family member or close friend
- How to behave with someone who is depressed
- What to do if someone is suicidal
- Self care for carers
- Key points to remember
- Further information and support
Someone with a mood disorder is like anyone with any other illness – they need care and support.
Family and friends can provide better care if they are informed about the illness, understand the type of treatment and are aware of the expected recovery time.
How to tell if someone has a mental illness
Even if you know someone well, you will not always notice when they have changed. You are more likely to notice big or sudden changes but gradual changes can be easy to miss. It’s also true that people will not always reveal all their thoughts and feelings to their close friends and family.
For these reasons, family and friends cannot expect to always know when someone has a depressive illness and should not feel guilty that they ‘did not know’.
The best approach is to acknowledge that mental illnesses are common and to learn how to recognise the signs and how to offer help.
What to do if you are concerned about a family member or close friend
If you are worried that a family member or close friend has a mood disorder, try talking to them about it in a supportive manner and either suggest that they consult their doctor or another mental health professional.
Sometimes they may be reluctant to seek help. You might need to explain why you’re concerned and provide specific examples of their actions or behaviour that are worrying you. Providing them some information such as a book, fact sheets or helpful pamphlets might also help.
You could offer to assist them in seeking professional help by:
- Finding someone that they feel comfortable talking to.
- Making an appointment for them on their behalf.
- Taking them to the appointment on the day
- Accompanying them during the appointment if appropriate.
This level of help may be particularly appropriate if the person has a severe mood disorder such as psychotic depression or mania.
Young people, adolescents in particular, are vulnerable to mental health problems. If you are concerned about someone, try:
- Gently let them know you have noticed. changes and explain why you are concerned
- Find a good time to talk when there are no pressures or interruptions.
- Listen and take things at their pace
- Respect their point of view.
- Validate what they are experiencing, but don’t offer reassurance or advice too quickly
- Let them know that there is help available that will make them feel better.
- Encourage them to talk to a doctor or other health professional, and to find a trusted friend or family member that they can confide in.
There are also a range of services (e.g. telephone counselling and online resources) that are specifically designed for young people. You can find out more about what is provided in Hong Kong on the Coolminds website.
How to behave with someone who is depressed
Patience, care and encouragement from others are vital to a person who is experiencing depression. Someone experiencing depression is very good at criticising themselves and needs support from others, not criticism.
Clear and effective communication within the household or family is also important. Partners or families might find it helpful to see a psychologist during this time for their own support.
An episode of depression can provide an opportunity for family members to re-evaluate the important things in life and resolve issues such as grief or relationship difficulties.
Some Tips:
- Avoid suggesting to the person that they “cheer up” or “try to get over it”. This is unhelpful as it is likely to reinforce their feelings of failure or guilt.
- Another important part of caring is to help the treatment process – if medication has been prescribed, encourage the person to persist with treatment and to discuss any side effects with their prescribing doctor.
- The person may also need encouragement and help to get to their therapy appointments or complete any online therapy exercises they have been asked to do.
- During a depressive illness, counselling or psychotherapy often results in the person working through their life events and relationships; while this can be difficult for all concerned, friends and family should not try to steer the person away from these issues.
What to do if someone is suicidal
If someone close to you is suicidal or unsafe, try:
- Talking to them about it and encourage them to seek help.
- Remembering that if someone is feeling like their life is not worth living, they are experiencing overwhelming emotional distress.
- Helping the person to develop a safety plan involving trusted close friends or family members that can keep the person safe in times of emergency.
- Removing risks (e.g. take away dangerous weapons or items if that person is angry or out of control and threatening to disappear).
Self care for carers
(A carer is someone who provides support to a friend, family member, or neighbor in need of help because of their age, disability, or physical or mental health.)
- Carers are also likely to experience stress. Depression and hopelessness have a way of affecting the people around them.
- Therapy can release difficult thoughts and emotions in carers too. So, part of caring is for carers to look after themselves to prevent becoming physically run down and to deal with their internal thoughts and emotions.
- Treatment has a positive time as well; when the person starts to re-engage with the good things in life and carers can have their needs met as well.
Key points to remember
- If you are worried that someone is depressed or has bipolar disorder, try talking to them about it in a supportive manner and suggest that they see a mental health professional.
- If they don’t want to seek help, explain the reasons for concern and perhaps provide them with some relevant information.
- Young people are particularly vulnerable to depression.
- Patience, care and encouragement from others are all vital to the person who is depressed.
- If a loved one talks of suicide, encourage them to seek help immediately from a mental health professional.
- Depression can take a toll on carers and close family members – it is important for these people to take care of themselves as well.
Contact Us
Coolminds
Email: hello@coolmindshk.com
Black Dog Institute
Email: blackdog@blackdog.org.au
Where to get more help and support
Bilingual Web Resources
Mind Hong Kong – “Am I A Carer?”
Mind Hong Kong – “What Can Friends and Family Do To Help?”
Student Health Service – “Understanding Depression”
Student Health Service – “Emotional Health”
English-Only Web Resources
Reach Out: a web-based support for adolescents
Headspace online: help for young people
Bilingual Telephone Hotlines
Samaritans Hong Kong 24-hour hotline: 28960000
Samaritan Befrienders Hong Kong 24-hour hotline: 23892222
Suicide Prevention Services 24-hour hotline: 23820000
Suicide Prevention Services “Youth Link” hotline (available 2pm-2am): 2382 0777
Hospital Authority Mental Health 24-hour Hotline: 2466 7350
Social Welfare Department Hotline: 2343 2255
Chinese-Only Telephone Hotlines
Youth Outreach 24-hour hotline service: 90881023
The Hong Kong Federation of Youth Groups “Youthline” hotline (available Mon-Sat, 2pm-2am): 27778899

Resources
Depression in Adolescents & Young People
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to the Black Dog Institute for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to the Black Dog Institute’s website: www.blackdoginstitute.org.au
What this fact sheet covers:
- Signs of depression in adolescence
- Where to get help for an adolescent
- Key points to remember
- Where to get more information
Introduction
- A 2017 study by the Hong Kong Federation of Youth Groups found that of the 3,441 secondary school and university students surveyed, 51% displayed symptoms of depression and close to 40% experienced high levels of stress (7 on a scale of 10).
- According to research done by the University of Hong Kong, more than two-thirds of Hong Kong’s university students experience symptoms of mild to severe depression.
- The HKJC Centre for Suicide Research and Prevention observed that suicide rates for full-time students increased by 76% between 2012 and 2016.
- Onset of depression is typically around mid-to-late adolescence, and it is important to recognise the early warning signs and symptoms. Early intervention can often prevent the development of severe depressive illness.
Developmental Impact
- The teenage years are a time when individuals develop their identity and sense of self.
- If depression is left to develop, it can lead to isolation from family and friends, risk-taking behaviours such as inappropriate sexual involvements and drug and alcohol abuse.
- It can also impact on school performance and study, which can have downstream effects on later career or study options.
- Both biological and developmental factors contribute to depression in adolescence. If bipolar disorder or psychosis is suspected, an assessment by a health professional is recommended. See our Fact Sheet “Symptoms of Bipolar Disorder” for more information.
Signs of depression in an adolescent
- An adolescent who is depressed may not show obvious signs of depression.
- It is often hard to distinguish adolescent turmoil from depressive illness, especially when the young person is forging new roles within the family and struggling with independence, and having to make academic and career decisions.
Signs of a depressed mood include:
- Lowered self-esteem (or self-worth)
- Changes in sleep patterns, that is, insomnia (inability to sleep), hypersomnia (excessive sleep) or broken sleep
- Changes in appetite or weight
- Inability to control emotions such as pessimism, anger, guilt, irritability and anxiety
- Varying emotions throughout the day. For example, feeling worse in the morning and better as the day progresses.
- Reduced capacity to experience pleasure: inability to enjoy what’s happening now, not looking forward to anything with pleasure such as hobbies or activities.
- Reduced pain tolerance: decreased tolerance for minor aches and pains
- Poor concentration and memory
- Reduced motivation to carry out usual tasks
- Lowered energy levels
Where to get help for an adolescent
- If you think someone you are close to might be depressed, you should encourage them to seek advice from a professional. (At school – school counsellor, social worker. Outside school – doctor, counsellor, psychologist)
- The first step is to speak to a professional who can conduct an assessment, provide options and discuss the next steps to take.
- Other initial sources of help are school counsellors and trusted close family members to whom the young person feels comfortable talking.
- If the young person does not want to seek help, it is best to explain your concerns and to provide them with some information to read about depression.
- There are also some excellent websites designed for young people, as well as confidential online and telephone counselling services in both English and Chinese. Please see our list of services at the end of this fact sheet.
- It’s important for young people to know that depression is a common problem and that there are people who can help.
- If there is any mention of suicide this should be taken seriously, and immediate assistance is available by calling 999 or going directly to the nearest hospital.
Key points to remember
- A 2017 study by the Hong Kong Federation of Youth Groups found that of the 3,441 secondary school and university students surveyed, 51% displayed symptoms of depression and close to 40% experienced high levels of stress (7 on a scale of 10).
- Depression in young people is associated with social withdrawal, drops in performance at school, drug or alcohol use and engaging in risky behaviours.
- It can be hard to distinguish depression from adolescent turmoil; if depression is suspected, an assessment should be sought from a doctor or other mental health professional.
- Immediate help should be sought if a young person talks of suicide.
Contact Us
Coolminds
Email: hello@coolmindshk.com
Black Dog Institute
Email: blackdog@blackdog.org.au
Where to get more Information and Support
Mind Hong Kong – “What Is Depression?”
Student Health Service – “Understanding Depression”
Student Health Service – “Emotional Health”
Bilingual Telephone Hotlines
Samaritans Hong Kong 24-hour hotline: 28960000
Samaritan Befrienders Hong Kong 24-hour hotline: 23892222
Suicide Prevention Services 24-hour hotline: 23820000
Suicide Prevention Services “Youth Link” hotline (available 2pm-2am): 2382 0777
Hospital Authority Mental Health Direct hotline: 24667350
Chinese-Only Telephone Hotlines
Youth Outreach 24-hour hotline service: 90881023
The Hong Kong Federation of Youth Groups “Youthline” hotline (available Mon-Sat, 2pm-2am): 27778899

Resources
Self-Harm + Young People
This resource booklet has been localised for the Hong Kong context and translated to Traditional Chinese by Coolminds, a mental health initiative run by Mind HK and KELY Support Group. For more information on Coolminds, please visit www.coolmindshk.com
Thank you to Orygen for donating their resources and for allowing us to adapt this. For the original version of this resource, please refer to Orygen’s website: www.orygen.org.au
Self-harm is when someone deliberately hurts or mutilates their body without meaning to die, although death may still occur as a result of the self-harming behavior.
Self-harming is a behaviour and not in itself a diagnosable mental disorder. Self-harm often occurs in young people who experience depression, anxiety, behavioural problems (such as conduct disorder) and substance use.
Facts about self-harm:
- Not all people who self-harm are suicidal, but it can be a sign that they are thinking of suicide.
- Self-harm often begins during youth and can be a way of communicating how bad someone feels or a method of coping with intense pain or distress.
- Around 1 in 6 young people have engaged in self-harm at some point in their lives and around 1 in 15 during a 12-month period.
- Support and treatment can help a young person learn safer and more helpful strategies for managing their distress and increasing their coping skills.
- Treatment for an underlying mental health problem (e.g., depression, anxiety) can also help in reducing or stopping self-harming behaviours.
What to look for?
There are many different types of behaviours that can be considered self-harming. The most common behaviours include self-cutting (e.g. cutting of upper arms/wrists/thighs) and self-poisoning (e.g. deliberately swallowing excessive amounts of prescribed or illegal drugs). Young people may also engage in self-burning (e.g. using cigarettes or lighters to burn the skin).
There are other behaviours that are not formally considered to be self-harming behaviours but are “risk-taking” behaviours that can lead to personal harm. Some examples are train-surfing, driving at high speed, illegal drug use, or repetitive unsafe sexual practices despite knowing about safe sex practices.
What causes self-harming behaviours?
People self-harm for different reasons, and sometimes it can be difficult to put the reasons into words. In many instances when someone engages in self-harming behaviour, it is an attempt to relieve, control or express distressing feelings. Some people who self-harm may not know other ways of telling people about their emotional pain, and some may feel a sense of control over pain when they self-harm.
Research suggests some people are more at risk of self-harming. This includes people who have experienced emotional, physical or sexual abuse, or stressful and highly critical family environments, or experience mental ill-health, such as depression.
People self-harm for different reasons, and sometimes it can be difficult to put the reasons into words.
What can young people do if they are engaging in self-harm?
Try to talk to someone about it. Telling a trusted adult can help to make sure the young person is safe and that medical assistance is received, if needed. If a young person repeatedly engages in self-harming behaviours, it is best to get some psychological treatment (counselling). One aim of counselling is to help the young person to feel better and find safer and more helpful ways of coping. Young people who are having suicidal thoughts should see a professional or call their local hospital or a help line, such as Suicide Prevention Services “Youth Link” hotline (available 2pm-2am): 2382 0777 or Hospital Authority Mental Health 24-hour Hotline: 2466 7350. (For more Hong Kong hotlines please refer to ‘Further information’ section at the end of this article.)
Counselling usually involves helping to increase problem-solving, communication and coping skills. Sometimes this can take time, so it’s best for young people to keep at counselling even if they think it’s not helping the first couple of times. It can be difficult to accept counselling after self-harming because of feelings of guilt, anger, or shame. Trying to be open to counselling or support can assist young people in feeling less overwhelmed and stressed in the long run.
Helping a young person who self-harms
Some people just stop self-harming, others can continue in a way that minimises physical risks, and others can place themselves at risk of dying. Even when self-harming behaviours stop, young people can experience long-term consequences associated with shame, guilt or coping with physical reminders, such as scarring. The best way to help someone you know that is self- harming is to encourage and support them to seek professional help as early as possible, to try to prevent longer-term consequences and to get the right help for any underlying mental health problems. Some things to do are:
- Try to help the young person feel safe to discuss the self-harm.
- Try to remain calm and maintain an open attitude recognising the young person may feel ashamed of their actions.
- Don’t be critical or get angry when discussing these issues.
- Ask the young person whether they feel suicidal. Call your local hospital or mental health service if you think the young person is suicidal to get professional help. Remember that someone’s risk does not always stay the same, so it is best to check in with them regularly.
- Supporting someone who self-harms can be a stressful experience and getting support for yourself is also recommended.
Really worried?
Initial treatment involves dealing with any immediate medical complications of self-harm, if present. Call an ambulance (999) or take the person to the accident and emergency department of the nearest hospital if the person needs urgent medical attention.
The best way to help someone you know who’s self-harming is to encourage and support them to seek professional help.
The best way to help someone you know who’s self-harming is to encourage and support them to seek professional help.
Advice and referral
If you know a young person who is repeatedly self-harming and you are not sure what to do, contact someone with experience in this field and discuss the situation with them.
If a young person refuses referral for further support, you need to discuss your concerns with them. Family members may find it helpful to let the young person know that they respect the young person’s wishes, but that they also care about the young person and need to discuss their concerns with a professional.
Workers need to explain the boundaries of their relationship with the young person and the limits of confidentiality. If the young person continues to be at risk and requires more care than the worker feels capable of providing, the worker should discuss the situation with a colleague and refer to a mental health professional or service.
Further information
For further information regarding mental health, or for information in other languages, visit:
Australia / International
- www.orygen.org.au
- www.headspace.org.au
- www.reachout.com
- www.youthbeyondblue.com
- www.beyondblue.org.au
- www.betterhealth.vic.gov.au
- www.sane.org
- www.healthdirect.gov.au
- www.oyh.org.au
Hong Kong
Bilingual Telephone Hotlines
- Samaritans Hong Kong 24-hour hotline: 28960000
- Samaritan Befrienders Hong Kong 24-hour hotline: 23892222
- Suicide Prevention Services 24-hour hotline: 23820000
- Suicide Prevention Services “Youth Link” hotline (available 2pm-2am): 2382 0777
- Hospital Authority Mental Health 24-hour Hotline: 2466 7350
- Social Welfare Department Hotline: 2343 2255
- Chinese-Only Telephone Hotlines
- Youth Outreach 24-hour hotline service: 90881023
- The Hong Kong Federation of Youth Groups “Youthline” hotline (available Mon-Sat, 2pm-2am): 27778899
Disclaimer: This information is not medical advice. It is generic and does not take into account your personal circumstances, physical wellbeing, mental status or mental requirements. Do not use this information to treat or diagnose your own or another person’s medical condition and never ignore medical advice or delay seeking it because of something in this information. Any medical questions should be referred to a qualified healthcare professional. If in doubt, please always seek medical advice.